Every year, over 1.3 million medication errors happen in the U.S. - and nearly a quarter of them come from simple mistakes on your prescription label. You pick up your pills, glance at the tiny print, and walk out. But what if that label says "take one daily" and you thought it meant "take one three times a day"? Or what if the medicine needs to be refrigerated, but you left it on the counter for two weeks? These aren’t rare accidents. They’re preventable - if you know what to ask.
What’s on the label - and what’s missing
A prescription label isn’t just a sticker. It’s a legal document with nine mandatory pieces of information: your name, the prescriber’s name, the drug’s brand and generic name, strength, dosage form, quantity, directions for use, number of refills, and the pharmacy’s contact info. That’s the baseline. But here’s the problem: labels can be cluttered, inconsistent, and hard to read. One study found only 42% of U.S. patients correctly understood their labels. Compare that to Germany, where standardized formatting helped 63% get it right.
Some labels bury critical details - like storage instructions - on the back in 8-point font. A patient in a 2023 Consumer Reports survey didn’t realize their blood pressure medicine needed refrigeration until they’d left it at room temperature for two weeks. That’s not negligence - it’s poor design. The FDA requires this information, but doesn’t enforce how it’s displayed. That’s why asking questions matters more than ever.
Ask: Is this the right medicine for me?
Never assume the pill looks right. Many drugs come in similar shapes and colors. A patient once took a diabetes pill thinking it was their cholesterol medicine - because both were small, white, and round. The generic name might be different from what your doctor said. Ask: "Is this the same as the one I took before?" Check the color, shape, and imprint code (the letters or numbers stamped on the pill). If it looks different, don’t take it until you confirm.
Also, ask if this is the brand or generic version. Sometimes, the pharmacy switches without telling you. That’s legal - but not always safe. Some people react differently to generics. If you’ve had side effects before, say so. Your pharmacist can check if the new version has the same active ingredient and dosage.
Ask: What are the exact directions?
"Take one by mouth" sounds simple. But what does "by mouth" mean? Can you crush it? Should you take it with food? On an empty stomach? Some meds need to be taken with a full glass of water. Others can’t be taken with dairy, grapefruit juice, or alcohol. For example, antibiotics like tetracycline lose effectiveness if taken with milk. Blood thinners like warfarin interact with leafy greens. If the label says "take as directed," ask for the exact schedule: "Is it once a day, every morning? Or every 12 hours?"
Abbreviations like "q.d." (once daily), "b.i.d." (twice daily), or "q.i.d." (four times daily) are common on labels - but many people don’t know them. Ask the pharmacist to spell it out in plain English. Repeat the instructions back to them. If they nod and say "yes," you’re more likely to remember correctly.
Ask: How should I store this?
Most medicines - 78% - are fine at room temperature (68-77°F). But 15% need refrigeration. That includes insulin, some antibiotics, and certain biologics. Leaving them out can make them useless - or dangerous. A 2022 survey found 1 in 5 patients didn’t know their meds needed cold storage. Ask: "Does this need to be kept in the fridge?" Then ask where in the fridge. Some medicines can’t go in the door (where it’s warmer) or near the freezer. If you’re unsure, ask for a printed storage guide.
Also ask: "Does it need to stay in its original bottle?" Some pills lose potency if moved to a pill organizer. Others are sensitive to light or moisture. If you’re traveling, ask for tips on keeping it safe on the road.

Ask: When does this expire?
Expiration dates aren’t suggestions. They’re science-backed deadlines. The FDA requires drugs to stay potent until that date - if stored correctly. But many people keep old meds for "just in case." That’s risky. Antibiotics past their date won’t kill bacteria - they might make infections worse. Some pills, like nitroglycerin for heart conditions, can become ineffective within months. Always check the expiration date. If it’s expired, ask if you need a new prescription. Don’t risk it.
Ask: Are there any serious side effects I should watch for?
Not all side effects are the same. Some are annoying - like drowsiness or dry mouth. Others are emergencies - like swelling, trouble breathing, or chest pain. Ask: "What are the red flags?" For example, if you’re on an opioid, you need to know the signs of an overdose: slow breathing, confusion, unresponsiveness. If you’re on an antidepressant, you should know about serotonin syndrome - high fever, fast heartbeat, agitation.
For high-risk drugs - like blood thinners, insulin, or chemotherapy - the FDA requires a separate Medication Guide. Ask for it. It’s not optional. These guides explain risks in plain language. If they don’t give you one, ask why. There are 107 medications that legally require this guide. If you’re on one, you deserve to know what to watch for.
Ask: Can I take this with my other meds or supplements?
Most people take multiple pills. The average American on prescription meds takes four. But interactions are silent killers. St. John’s Wort can make birth control fail. Calcium supplements can block thyroid meds. Even over-the-counter painkillers like ibuprofen can raise blood pressure if you’re on ACE inhibitors. Give your pharmacist your full list - including vitamins, herbal remedies, and CBD. They can spot clashes you didn’t know existed.
Ask: "Is there anything I should avoid while taking this?" That includes alcohol, caffeine, sunlight (some meds cause sunburn), and even certain foods. Don’t guess. Ask.

Ask: How many refills do I have - and when do I need to reorder?
Running out of medicine is a common cause of treatment failure. If you’re on a monthly pill, you should refill at least 3-5 days before you run out. But refills aren’t always obvious. Some labels say "Refills: 3" - but your insurance might only cover 2. Others say "No refills" - but your doctor didn’t say that. Ask: "How many refills are left?" and "Do I need a new prescription after this?"
If you’re on Medicare Part D, your coverage might change mid-year. Some plans limit refills during the "donut hole." Ask your pharmacist if your refill will be covered. If not, ask if there’s a cheaper alternative or if you qualify for a patient assistance program.
Ask: Is there a simpler way to understand this?
If the label is too small, too confusing, or written in a language you don’t understand - ask for help. You have rights. By law, pharmacies that get federal funding must provide free translation services. Ask for a Spanish, Mandarin, Arabic, or any other language version. You can also ask for a large-print label - 92% of U.S. pharmacies offer this.
Many pharmacies now use QR codes on labels. Scan it with your phone and watch a short video explaining how to take the medicine. Some even use augmented reality - point your phone at the bottle and see dosage instructions float on top of it. Ask: "Do you have a video or app for this medication?" If they say no, ask if they plan to offer it. Demand better tools. You’re not asking for luxury - you’re asking for safety.
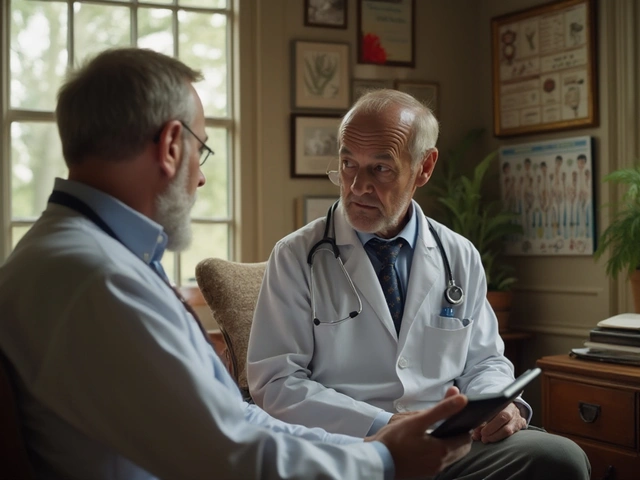
What if something still feels off?
Trust your gut. If the label doesn’t match what your doctor told you, if the pill looks wrong, if the instructions seem unclear - don’t take it. Go back. Call your doctor. Call the pharmacy again. Ask to speak to the pharmacist, not just the technician. You have every right to double-check. The Institute for Safe Medication Practices says verifying the "5 Rights" - Right Patient, Right Medicine, Right Dose, Right Route, Right Time - cuts errors by nearly 60%.
And if you’re ever unsure, use the FDA’s free "Medication Check-Up" program. It’s available at over 8,400 pharmacies. A trained staff member will sit with you, go over your labels, and answer your questions - no charge, no appointment needed.
Why this matters more than you think
Medication errors don’t just cause discomfort. They send 1.3 million people to the ER each year. They lead to hospitalizations, organ damage, and even death. The cost? $1.4 billion a year in avoidable healthcare spending. But here’s the good news: when patients ask questions, adverse events drop by 47%. That’s not magic. That’s power.
Pharmacies are under pressure. They’re busy. Labels are messy. Systems are outdated. But you’re not powerless. You hold the final checkpoint. You’re the last line of defense between a dangerous mistake and your health. Don’t be polite. Don’t be shy. Ask. Repeat. Confirm. You’re not being difficult - you’re being smart.
What should I do if my prescription label looks different from last time?
Don’t assume it’s a mistake. First, check the generic name - pharmacies often switch brands to save costs. Compare the pill’s color, shape, and imprint code with your previous prescription. If it doesn’t match, ask the pharmacist: "Is this the same medicine?" If they confirm it’s a different brand or generic, ask if it will work the same way for you. If you’ve had side effects before, say so. You have the right to request your original brand if it’s medically necessary.
Can I get my prescription label in large print or another language?
Yes. By law, pharmacies that receive federal funding (including most major chains) must provide free translation services and large-print labels upon request. Ask the pharmacist for a large-print version or a label in your preferred language. You can also ask for a printed Medication Guide in your language - especially if you’re on a high-risk drug like insulin or an opioid. Most pharmacies have these available or can order them within 24 hours.
What if the pharmacy gives me the wrong medicine?
If you realize you were given the wrong medicine, don’t take it. Return to the pharmacy immediately. Ask to speak to the pharmacist, not just the technician. Report the error clearly: "This is not the medication I was supposed to get." The pharmacy is required to document the mistake and notify the prescriber. You can also report it to the FDA’s MedWatch program online or by phone. Mistakes happen - but reporting them helps prevent them for others.
Do I need to ask about drug interactions even if I only take one prescription?
Yes. Even if you only take one prescription, you likely take other things - vitamins, supplements, over-the-counter pain relievers, or even herbal teas. St. John’s Wort, for example, can interfere with antidepressants, birth control, and blood thinners. Calcium supplements can block thyroid meds. Even grapefruit juice can make some cholesterol drugs dangerously strong. Always list everything you take - including what you take occasionally - when you pick up your prescription. The pharmacist can spot hidden risks.
How do I know if my prescription needs refrigeration?
Look for symbols on the label - a snowflake or "Refrigerate" in bold text. If it’s not clear, ask: "Does this need to be kept cold?" Some medicines, like insulin, certain antibiotics, and biologics, must be refrigerated. If stored at room temperature, they can lose potency. If you’re unsure, ask the pharmacist to show you the storage instructions on the Medication Guide or label. When in doubt, keep it cold until you confirm.