TCA Comparison Tool
Tricyclic Antidepressant Comparison
Compare key characteristics of first-generation TCAs used in depression treatment.
Key Differences
Important Safety Note
Tricyclic antidepressants carry overdose risks including cardiac toxicity. Always follow prescribed dosing. See full safety information
When talking about the birth of modern antidepressants, Imipramine is a synthetic tricyclic compound first synthesized by the Swiss firm Ciba in the late 1950s, later marketed as Tofranil. Its story is a mix of serendipity, rigorous clinical trials, and a shift in how psychiatry viewed mood disorders.
Key Takeaways
- Imipramine was discovered by Ciba in 1957 while looking for antihistamines.
- Clinical observations in the early 1960s revealed powerful antidepressant effects.
- It launched the class of tricyclic antidepressants (TCAs) and changed psychiatric practice.
- Regulatory approval, marketing under the name Tofranil, and subsequent safety concerns shaped its legacy.
- Modern research still revisits imipramine to understand antidepressant mechanisms.
Early Chemical Roots
The parent structure of imipramine is a dibenzazepine ring system. Chemists at Ciba, led by Roland Wermuth, were tasked with creating new antihistamines after the success of diphenhydramine. In 1957 they synthesized a series of compounds coded CIBA 411‑1, CIBA 411‑2, etc. One of those, later named imipramine, showed a surprisingly strong effect on the central nervous system.
From Antihistamine to Mood Lifter
Initial animal tests suggested the compound could cross the blood‑brain barrier. When physicians started using it off‑label for insomnia, patients reported lifted mood and increased energy. The turning point came in a small study at the British Journal of Psychiatry, where six depressed volunteers showed dramatic improvement after two weeks of treatment. The study sparked a wave of interest across Europe and North America.
Clinical Trials and FDA Approval
By 1960, Ciba partnered with Smith, Kline & French (later part of GlaxoSmithKline) to run larger, multi‑center trials. The data demonstrated a 70% response rate in patients with major depressive disorder, far surpassing the placebo response of 20‑30% typical at the time.
In 1961 the U.S. Food and Drug Administration (FDA) granted approval for the brand name Tofranil. It became the first antidepressant marketed in the United States, paving the way for an entire therapeutic class.

How Imimprine Works - A Snapshot of Neurochemistry
Imipramine belongs to the tricyclic antidepressants (TCAs) family. Its primary mechanism is the inhibition of reuptake for two key neurotransmitters: serotonin and norepinephrine. By blocking the transporter proteins that normally pull these chemicals back into neurons, imipramine raises their extracellular levels, which correlates with mood improvement.
Beyond the serotonin‑norepinephrine axis, the drug also exerts antihistaminic and anticholinergic effects, explaining side‑effects like dry mouth, sedation, and orthostatic hypotension. These off‑target actions made clinicians cautious but also gave the drug utility in treating chronic pain and certain types of anxiety.
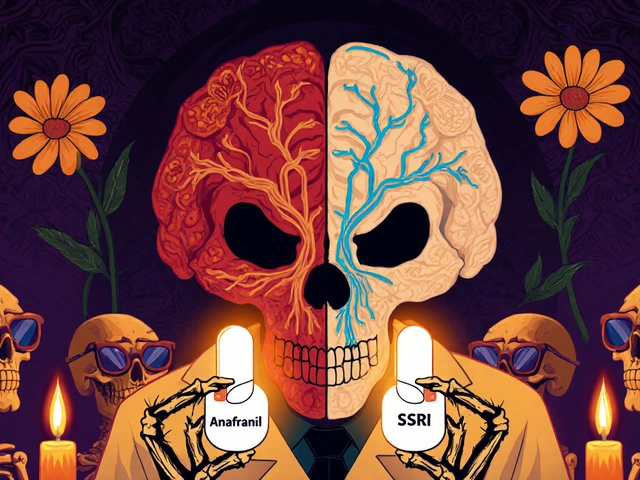
Comparison with Early TCAs
| Attribute | Imipramine (Tofranil) | Amitriptyline (Elavil) | Desipramine (Norpramin) |
|---|---|---|---|
| Year of launch | 1961 (US) | 1961 (US) | 1962 (US) |
| Primary reuptake inhibition | Serotonin & Norepinephrine | Serotonin & Norepinephrine | Norepinephrine (stronger) |
| Anticholinergic side‑effects | Moderate | High | Low |
| Typical dose range (mg/day) | 150‑300 | 75‑150 | 75‑200 |
The table shows why imipramine quickly became the “starter” TCA: a balanced neurotransmitter profile and a tolerable side‑effect spectrum compared with amitriptyline, which was notorious for strong anticholinergic actions.
Impact on Psychiatric Practice
Before imipramine, depression was largely treated with electroconvulsive therapy (ECT) or with sedating barbiturates that offered little mood benefit. The drug’s success sparked a paradigm shift: depression could be managed pharmacologically, allowing outpatient treatment and reducing hospitalization rates. By the mid‑1970s, TCAs were the cornerstone of depression treatment worldwide.
The widespread adoption also brought challenges. Overdose risk, due to cardiac toxicity, forced the emergence of new safety protocols and spurred the search for safer agents, ultimately leading to the development of selective serotonin reuptake inhibitors (SSRIs) in the 1980s.
Modern Re‑evaluation and Current Use
Even with newer antidepressants, imipramine remains on formularies for specific indications:
- Treatment‑resistant depression where SSRIs failed.
- Nocturnal enuresis in children - the drug reduces nighttime urine production.
- Certain chronic pain syndromes, exploiting its antihistaminic properties.
Recent pharmacogenomic studies suggest that patients with specific CYP2D6 genotypes metabolize imipramine slower, requiring dose adjustments. This precision‑medicine angle keeps the drug relevant in academic circles.
Key Lessons from the Imipramine Story
- Serendipity matters. A compound aimed at allergies turned into a landmark antidepressant.
- Rigorous clinical observation can uncover hidden therapeutic potentials.
- Regulatory pathways and branding (Tofranil) are crucial for market adoption.
- Safety concerns drive innovation - imipramine’s toxicity led directly to the rise of SSRIs.
- Even older drugs can find new roles when re‑examined with modern science.
Frequently Asked Questions
When was imipramine first synthesized?
Imipramine was first synthesized in 1957 by chemists at the Swiss company Ciba.
What brand name is imipramine sold under?
The most widely recognized brand name is Tofranil.
How does imipramine differ from amitriptyline?
Both are TCAs, but imipramine has a more balanced serotonin‑norepinephrine blockade and milder anticholinergic side‑effects compared with amitriptyline’s stronger anticholinergic profile.
Is imipramine still prescribed today?
Yes, especially for treatment‑resistant depression, nocturnal enuresis in children, and certain chronic pain conditions, though it’s prescribed less often than newer agents.
What are the main side‑effects to watch for?
Common side‑effects include dry mouth, constipation, sedation, orthostatic hypotension, and in overdose situations, cardiac arrhythmias.
Understanding the journey of imipramine-from a lab curiosity to a therapeutic milestone-offers a clear window into how modern psychopharmacology evolved. Its legacy lives on, reminding clinicians and researchers that breakthroughs often arise from unexpected places.