Many people carry a label in their medical record: sulfa allergy. It sounds simple - avoid anything with "sulfa." But here’s the problem: that label might be wrong, and worse, it could be keeping you from safe, effective medications you actually need.
Let’s cut through the confusion. A true sulfa allergy isn’t about sulfur. It’s not about sulfates in Epsom salts, sulfites in wine, or saccharin in diet soda. It’s about a very specific chemical structure found in only one class of drugs: antibiotic sulfonamides. These include sulfamethoxazole (in Bactrim or Septra), sulfadiazine, sulfacetamide, and dapsone. If you had a reaction to one of these - like a rash, fever, or worse, Stevens-Johnson Syndrome - then yes, you should avoid them. But if your doctor says you can’t take hydrochlorothiazide for high blood pressure or furosemide for fluid retention because of a "sulfa allergy," that advice is outdated and potentially harmful.
What’s Really Going On With Sulfa Allergies?
About 3% of people say they have a sulfa allergy. But studies show only 1.5-2% actually have a confirmed IgE-mediated reaction. The rest? Many had side effects like nausea or a mild rash that wasn’t an allergy at all. Others were misdiagnosed after a viral infection mimicked an allergic reaction. The result? Millions of people live with a label that limits their treatment options unnecessarily.
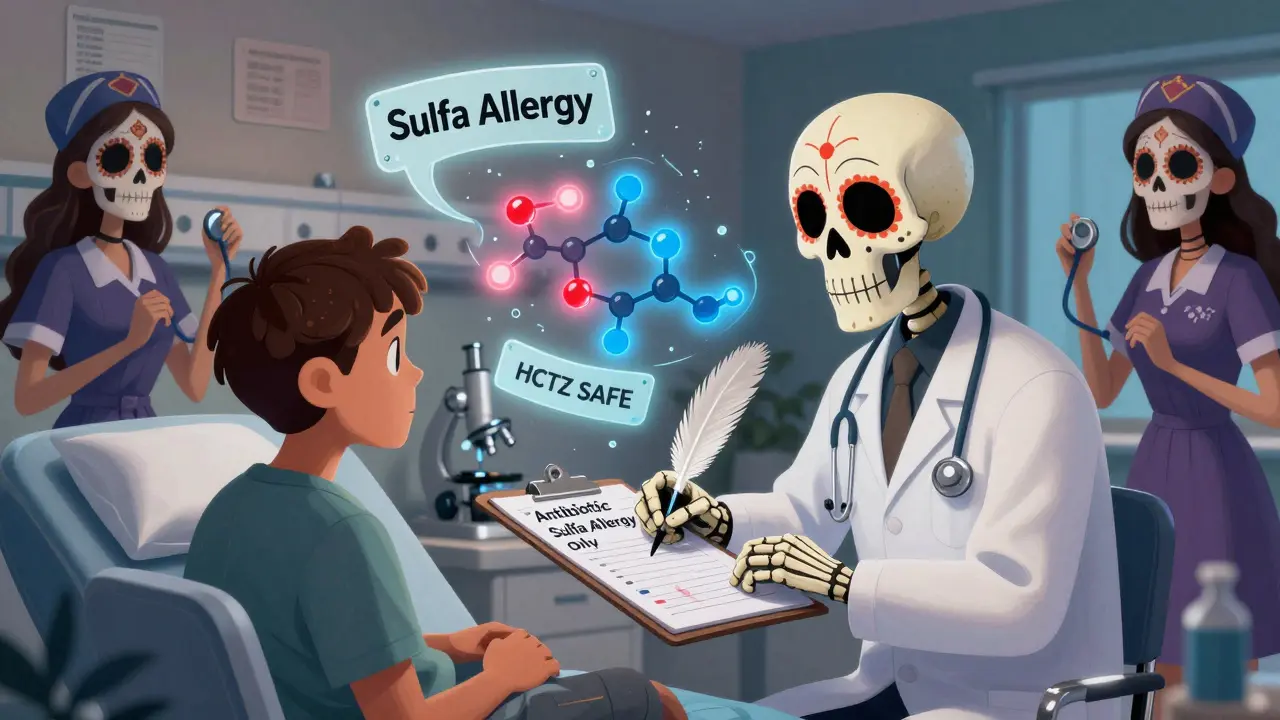
The key lies in molecular structure. Antibiotic sulfonamides have a unique part called an arylamine group at the N4 position. When the body breaks them down, it creates a reactive compound called hydroxylamine. That’s what triggers the immune response in true allergies. Non-antibiotic sulfonamides - like furosemide (Lasix), hydrochlorothiazide (HCTZ), celecoxib (Celebrex), and acetazolamide - don’t have this group. Their chemistry is different. And because of that, they don’t cross-react.
Which Medications Are Safe?
Here’s the practical breakdown:
- AVOID: Sulfamethoxazole-trimethoprim (Bactrim, Septra), sulfadiazine, sulfacetamide (eye drops), dapsone (used for leprosy and some skin conditions).
- SAFE: Furosemide (Lasix), hydrochlorothiazide (HCTZ), chlorthalidone, celecoxib (Celebrex), sulfonylureas like glyburide (for diabetes), acetazolamide (for glaucoma or altitude sickness), and metolazone.
There’s one exception: sulfasalazine (Azulfidine). It’s used for rheumatoid arthritis and ulcerative colitis. About 10% of people with a true antibiotic sulfa allergy react to it - because it breaks down into sulfapyridine, which does have the arylamine group. So if you’re on sulfasalazine and have a history of sulfa allergy, talk to your doctor before continuing.
A 2019 review of over 1,200 patients with confirmed sulfonamide antibiotic allergy found only 0.8% reacted to non-antibiotic sulfonamides - the same rate as people with no allergy at all. That’s not a risk. That’s noise.
Why This Misunderstanding Costs Lives and Money
When doctors avoid hydrochlorothiazide because of a "sulfa allergy," they often switch to a different blood pressure pill - maybe a calcium channel blocker or an ACE inhibitor. Those can be fine, but they’re not always better. Some carry higher risks of side effects like cough, swelling, or kidney changes. Worse, if someone needs a diuretic for heart failure and can’t take furosemide, their condition can worsen.
It’s even worse in hospitals. A 2022 report from the Patient Safety Network found that 12.3% of antibiotic selection errors in hospitalized patients came from unnecessary sulfa allergy labels. Instead of using Bactrim - a narrow-spectrum, low-cost drug - doctors gave broader antibiotics like levofloxacin or vancomycin. Those drugs increase the risk of C. difficile infection by over two-fold. That means longer hospital stays, higher costs, and more complications.
The financial toll? An estimated $1.2 billion a year in the U.S. alone. That’s from extra medications, longer stays, and avoidable infections. And it’s all because of a misunderstanding.
How to Fix Your Allergy Label
If you’ve been told you have a sulfa allergy, here’s what to do:
- Ask: What reaction did I have? Was it a mild rash? Or something serious like blistering skin, fever, or trouble breathing? Mild rashes are rarely true allergies.
- Check your records. Does your chart just say "sulfa allergy"? Ask for clarification: "Was it an antibiotic?" If it’s vague, request a review.
- Consider a challenge. If your reaction was mild and happened years ago, your doctor can do a supervised test. Give you a single dose of hydrochlorothiazide or furosemide and watch for 24-48 hours. In Macy’s 2019 study, 98.7% of patients passed this test without issue.
- Update your records. If you’re cleared, ask your provider to change "sulfa allergy" to "sulfonamide antibiotic allergy" - or remove it entirely if no real reaction occurred.
Pharmacists are key here. A 2021 study found that when pharmacists proactively reviewed allergy lists, they reduced unnecessary restrictions by 68.4%. They caught errors like patients being denied glaucoma drops or diabetes meds because of a 20-year-old rash.
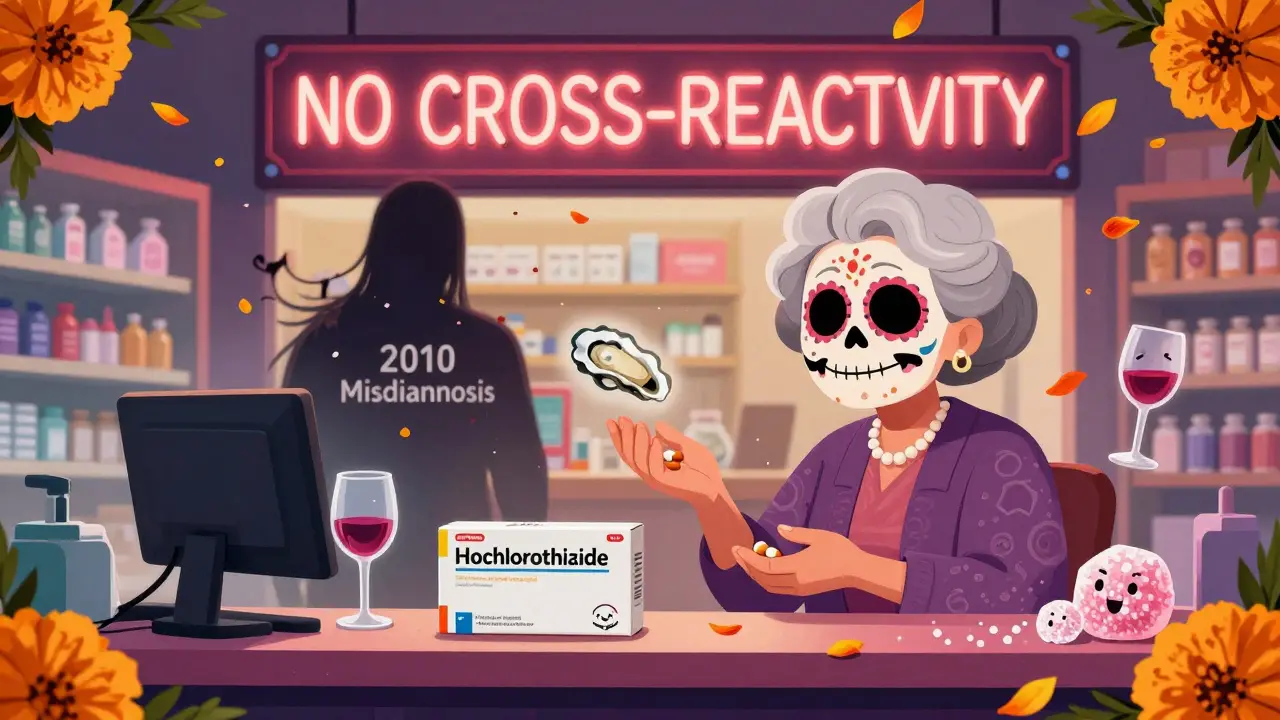
What About Other Sulfur-Containing Things?
You’ve probably heard: "If you’re allergic to sulfa, avoid seafood, sulfites, or Epsom salts." That’s a myth. Sulfur is everywhere. It’s in your body. It’s in amino acids. Sulfates (like magnesium sulfate in Epsom salts) are chemically unrelated to sulfonamides. Sulfites (used as preservatives) are different too. No cross-reactivity. No risk. You can eat oysters. You can drink wine. You can soak in Epsom salts. None of these will trigger a reaction if your allergy is to antibiotics.
What’s Changing in 2026?
Health systems are finally catching up. Epic Systems, used by 63% of U.S. hospitals, now has built-in alerts that distinguish between antibiotic and non-antibiotic sulfonamides. When a doctor tries to order furosemide for someone with a "sulfa allergy," the system now says: "No cross-reactivity. Safe to use." Cerner is rolling out similar updates in 2025.
The FDA updated its drug labeling guidelines in 2021, requiring manufacturers to clearly separate antimicrobial from non-antimicrobial sulfonamides. The American Academy of Allergy, Asthma & Immunology now explicitly states there’s no clinically significant cross-reactivity. And the Joint Commission added a new patient safety goal in 2024: accurate allergy documentation.
Still, 67% of primary care doctors in a 2023 survey believed non-antibiotic sulfonamides should be avoided. That’s why education matters. A single 10-minute conversation with your doctor or pharmacist can change your treatment path.
Real Stories, Real Impact
One patient in Calgary, 68, had been told she couldn’t take her blood pressure med for 12 years because of a "sulfa allergy" from a childhood rash. She was on a more expensive, less effective drug. After a simple challenge, she switched back to hydrochlorothiazide. Her blood pressure stabilized. Her out-of-pocket costs dropped by $800 a year.
Another man with heart failure was denied furosemide twice because his chart said "sulfa allergy." He ended up in the ER with fluid overload. When his cardiologist dug deeper, they found his only reaction was to Bactrim - and he’d taken HCTZ safely for 15 years before that label got added.
These aren’t rare. They’re routine.
Is a sulfa allergy the same as being allergic to sulfur?
No. A sulfa allergy is a reaction to a specific chemical structure found only in certain antibiotic drugs. Sulfur is a natural element found in many foods, supplements, and compounds like sulfates and sulfites. These have nothing to do with sulfa drugs. You can safely consume sulfur-containing foods, use Epsom salts, or drink wine even if you have a true sulfa allergy.
Can I take hydrochlorothiazide if I have a sulfa allergy?
Yes. Hydrochlorothiazide (HCTZ) is a non-antibiotic sulfonamide. It lacks the arylamine group that causes allergic reactions in antibiotic sulfonamides. Multiple studies show no increased risk of reaction. If you’ve been told to avoid it, ask your doctor about a supervised challenge - most people tolerate it without issue.
What if I had a severe reaction like Stevens-Johnson Syndrome?
If you had a life-threatening reaction like SJS, TEN, or DRESS to a sulfonamide antibiotic, you should avoid all other antimicrobial sulfonamides. But non-antibiotic sulfonamides like furosemide, celecoxib, or HCTZ are still safe. The immune response is specific to the antibiotic structure. Always discuss this with an allergist before making decisions.
Why do some doctors still say to avoid all sulfa drugs?
Because the misinformation has been around for decades. Many providers were taught that all "sulfa" drugs cross-react. Electronic health records often don’t distinguish between types. But current evidence is clear: cross-reactivity only happens within antibiotic sulfonamides. Major organizations like the AAAAI, Mayo Clinic, and FDA now recommend clear labeling and safe use of non-antibiotic sulfonamides.
How can I get my allergy label corrected?
Start by talking to your primary care provider or pharmacist. Ask: "Was my reaction to an antibiotic?" If it was mild and happened long ago, request a supervised challenge with a non-antibiotic sulfonamide like HCTZ. If cleared, ask them to update your record to say "sulfonamide antibiotic allergy" or remove it entirely. Bring printouts of current guidelines - they’re widely available from the AAAAI and CDC.