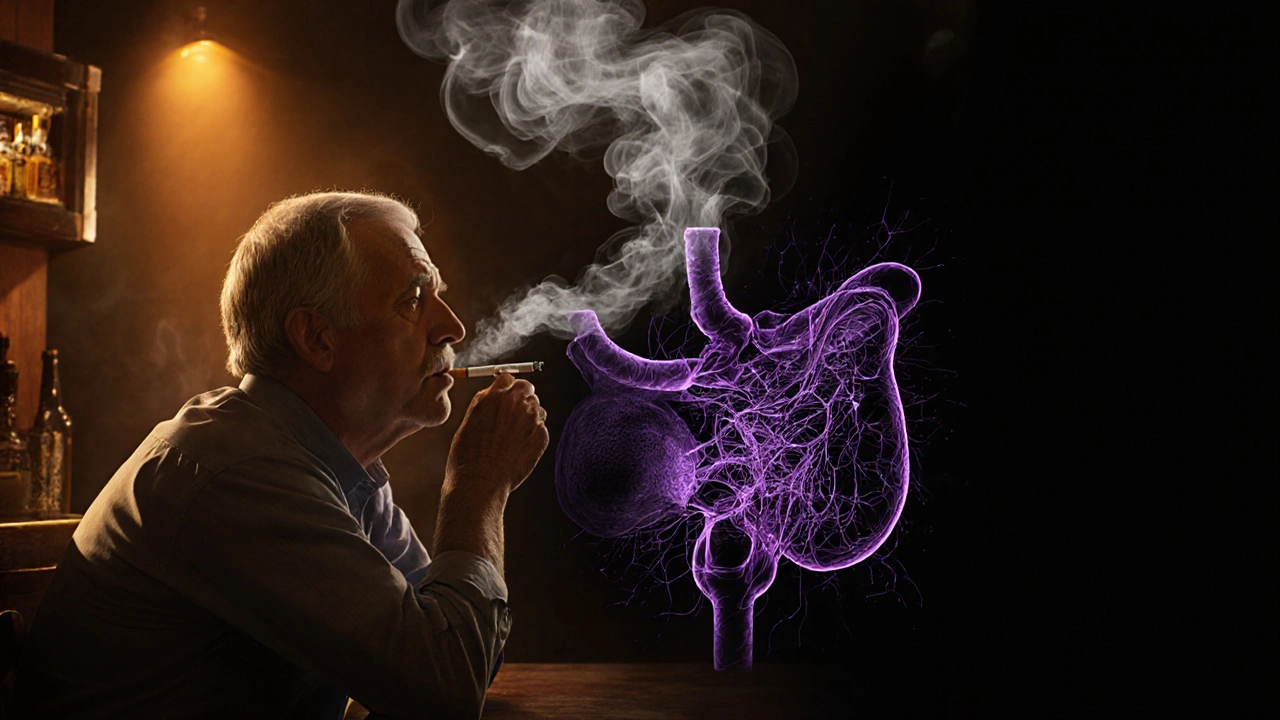
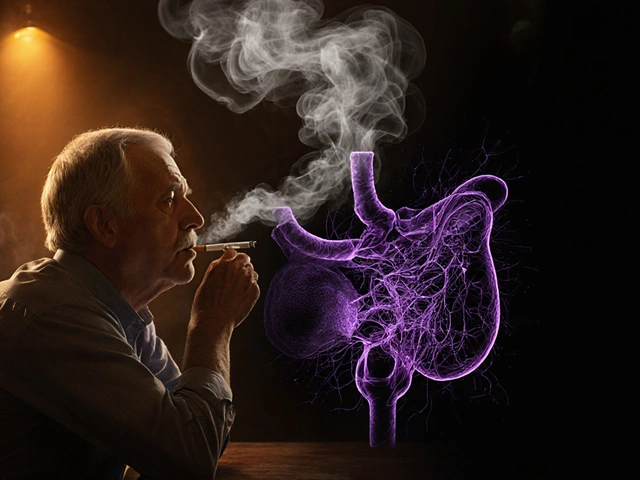
Pancreatic cancer is a malignant disease of the pancreas that often goes undetected until advanced stages, characterized by a 5‑year survival rate of roughly 10%. When combined with smoking the inhalation of tobacco smoke containing thousands of chemicals, the odds of developing this deadly disease jump dramatically. This article breaks down the science, numbers, and practical steps you can take to lower your risk.
Why Tobacco is a Potent Carcinogen for the Pancreas
Every puff delivers more than 70 known carcinogens substances that can damage DNA and trigger cancer. Among them, nitrosamines highly reactive chemicals formed during tobacco curing are especially harmful to pancreatic tissue. Once absorbed, they travel through the bloodstream, settle in the pancreas, and cause mutations in key genes such as KRAS an oncogene that drives uncontrolled cell growth when altered.
Beyond direct DNA damage, nicotine-a major component of tobacco-stimulates inflammation. Chronic inflammation creates an environment where precancerous cells thrive, often manifesting as chronic pancreatitis long‑term inflammation of the pancreas that increases cancer risk. The combined assault of carcinogens and inflammation explains why smokers face a 2‑ to 3‑fold higher risk of pancreatic cancer compared to never‑smokers.
Statistical Snapshot: Smoking‑Related Risk
Large‑scale studies, such as those cited by the World Health Organization the UN agency that monitors global health trends, show a clear dose‑response curve:
- Current smokers have an relative risk of 1.7-2.0 for pancreatic cancer.
- Former smokers who quit more than 10years ago see their risk fall close to that of never‑smokers.
- Each pack‑year (one pack per day for one year) adds roughly a 5% increase in lifetime risk.
In Canada, annual pancreatic cancer deaths among smokers account for about 30% of all cases, according to the Canadian Cancer Society.
How Smoking Interacts with Other Risk Factors
Smoking rarely acts alone. It amplifies the impact of diabetes, obesity, and hereditary predisposition. For example, individuals with type2 diabetes a chronic condition that raises blood sugar and inflammation levels who also smoke see a combined risk that can exceed a 4‑fold increase compared with non‑smokers without diabetes.
Comparing Risk: Smokers vs. Non‑Smokers
| Group | Relative Risk (RR) | 5‑Year Survival | Typical Age at Diagnosis |
|---|---|---|---|
| Never‑smokers | 1.0 (baseline) | ≈12% | 71years |
| Current smokers | 1.8-2.0 | ≈9% | 68years |
| Former smokers (quit≥10yrs) | 1.2 | ≈11% | 70years |

Key Takeaways
- Smoking roughly doubles the risk of pancreatic cancer.
- Carcinogens like nitrosamines and nicotine‑driven inflammation are the main culprits.
- Quitting reduces risk; benefits appear within a decade.
- Combined risk factors (diabetes, obesity) magnify the danger.
- Early screening is critical for high‑risk individuals.
Practical Steps to Lower Your Risk
- Quit smoking - use nicotine‑replacement therapy or prescription aids; seek support groups.
- Maintain a healthy weight - BMI under 25 lowers pancreatic stress.
- Control blood sugar - regular monitoring if you have diabetes.
- Limit alcohol intake - heavy drinking adds another layer of risk.
- Discuss screening with your doctor - especially if you have a family history of pancreatic or other GI cancers.
Remember, the greatest change you can make is to stop the source of carcinogens. Even reducing the number of cigarettes per day cuts exposure to harmful chemicals, and the body begins repairing DNA damage within weeks.
Related Topics to Explore
If you found this piece useful, you might also want to read about:
- “Pancreatic cancer screening guidelines” - what tests are recommended for high‑risk groups.
- “How diet influences pancreatic health” - foods that protect or harm the pancreas.
- “Managing nicotine addiction” - strategies to quit for good.
Frequently Asked Questions
Can occasional smoking still increase pancreatic cancer risk?
Yes. Even light or occasional smoking introduces carcinogens that can accumulate over time. Studies show a measurable risk rise after just 10-15 pack‑years, which can be achieved with intermittent use over many years.
How long does it take for risk to drop after quitting?
Risk begins to decline within the first five years and approaches the level of never‑smokers after about 10‑15 years of abstinence, according to longitudinal cohort data.
Is there a specific test to detect early pancreatic cancer in smokers?
Currently, no single screening test is universally recommended. High‑risk individuals (e.g., long‑term smokers with family history) may undergo endoscopic ultrasound (EUS) or MRI/MRCP under specialist guidance.
Do e‑cigarettes pose the same pancreatic risk?
Evidence is still emerging, but many of the same nitrosamine compounds appear in vapor. Until long‑term data is available, it’s safest to treat e‑cigarettes as a potential risk.
What lifestyle changes help after quitting smoking?
Focus on a balanced diet rich in fruits, vegetables, and whole grains; maintain regular physical activity; manage stress; and keep blood sugar and cholesterol in check. These habits support DNA repair and lower overall cancer risk.