When your heart arteries are clogged, two main options exist: PCI and CABG. Neither is "better" across the board. The right choice depends on your specific heart anatomy, health conditions, and what matters most to you-quick recovery or long-term peace of mind.
Imagine your coronary arteries as pipes feeding oxygen to your heart muscle. When they get blocked by plaque, your heart struggles. Two proven ways to fix this are Percutaneous Coronary Intervention (PCI), commonly called stenting, and Coronary Artery Bypass Grafting (CABG), or bypass surgery. Both work. But they work in very different ways, and the outcomes vary depending on who you are.
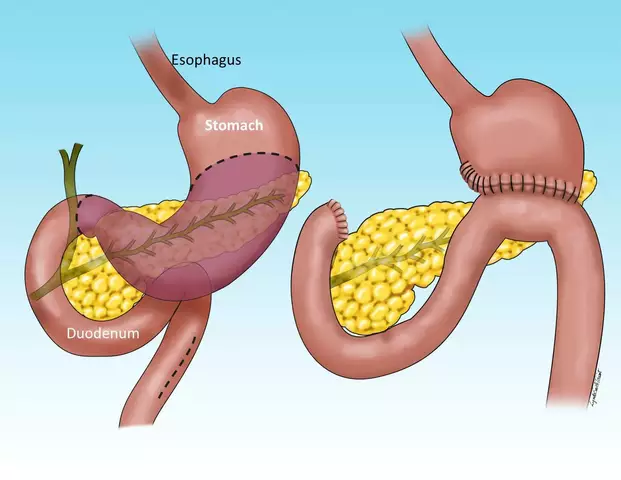
PCI is a minimally invasive procedure done in a cath lab. A thin tube is threaded through an artery in your wrist or groin, guided to the blocked coronary artery, and a small mesh tube-called a stent-is expanded to open the blockage. Most patients go home the next day. It’s quick. It’s common. In the U.S., about 600,000 PCIs are done every year.
CABG, on the other hand, is open-heart surgery. Surgeons take a healthy blood vessel-often from your chest, leg, or arm-and graft it around the blocked section of your coronary artery. This creates a new path for blood to flow. It’s a major operation. You’ll spend 5 to 7 days in the hospital and need 6 to 8 weeks to fully recover. Around 300,000 CABG surgeries are performed annually in the U.S.
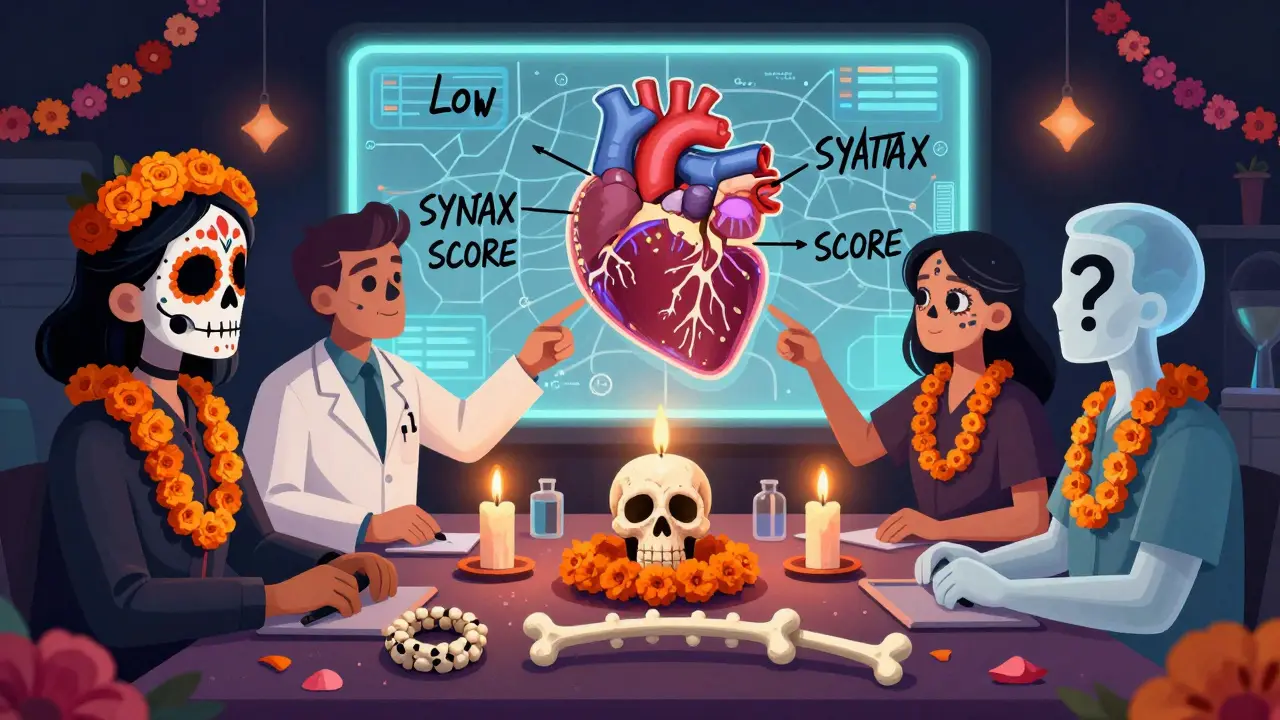
How doctors decide: The SYNTAX score and your heart’s map
Doctors don’t pick one over the other based on gut feeling. They use tools. One of the most important is the SYNTAX score. It’s a detailed analysis of your coronary angiogram that rates how complex your blockages are. Think of it like a road map of your heart’s arteries.
- If your SYNTAX score is below 22, PCI is usually the preferred choice.
- If it’s above 32, CABG is strongly recommended.
- If it’s between 22 and 32? That’s where things get personal.
Why does complexity matter? Simple blockages in one or two arteries respond well to stents. But if you have multiple blockages, especially in the left main artery or near the main pumping chamber, bypass surgery gives you a more durable fix. The data is clear: complex disease treated with stents has a much higher chance of needing another procedure later.
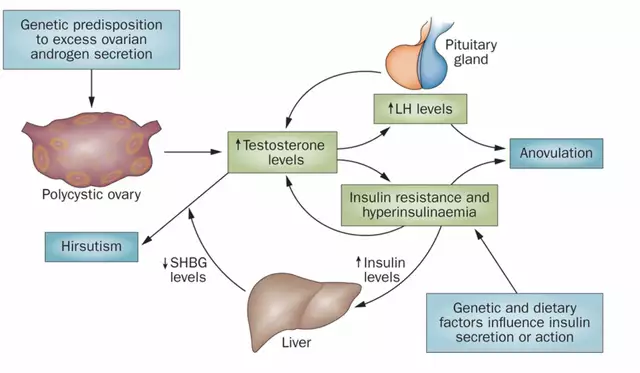
Diabetes changes everything
If you have diabetes and multivessel disease, this isn’t a close call. The FREEDOM trial, a landmark study involving over 1,900 diabetic patients, showed something startling: after five years, 16.4% of those who got stents had died. Only 10% of those who had bypass surgery had.
That’s a 6.4% absolute difference in survival. For diabetic patients, CABG isn’t just preferred-it’s a Class IA recommendation, meaning it’s the strongest possible guideline endorsement. Why? Because diabetes damages blood vessels in a way that makes stents more likely to re-narrow. Bypass grafts, especially those made from the internal mammary artery, last longer and resist plaque buildup better.
Left main disease: A turning point
Blockages in the left main coronary artery are dangerous. It’s the main highway feeding most of your heart. For years, bypass was the only accepted option. But newer stents changed the game.
The EXCEL trial showed that for patients with left main disease, PCI and CABG had similar outcomes at three years. But here’s the twist: the first 30 days favored PCI. After that, the advantage flipped. By five years, CABG had a 61% lower risk of major events like heart attack or repeat procedures.
Another study, the NOBLE trial, found that while death rates were similar, PCI patients were more than twice as likely to need another procedure. If you’re young and active, avoiding repeat interventions matters. CABG gives you that durability.
Recovery: Fast vs. lasting
Let’s be honest-most people want to get back to life fast. PCI wins here. Most patients are back to normal activities within a week. One patient on Reddit said, “Back to work in 3 days.” That’s real.
CABG recovery is harder. You’ll feel sore for weeks. Your sternum is cut open and wired back together. About 45% of patients still have chest pain at three months. But here’s what most don’t realize: by six months, 94% of both PCI and CABG patients are back at work. The long-term quality of life often favors CABG.
The ROSETTA trial found that one year after surgery, CABG patients reported better symptom relief and higher quality-of-life scores. One patient wrote: “Six weeks of recovery was tough, but two years later I’m hiking again with no chest pain.” That’s the kind of result that lasts.
The hidden risks: Stroke and repeat procedures
No procedure is risk-free. CABG carries a slightly higher risk of stroke-about 1.7% versus 1% for PCI. That’s because the heart is stopped and blood flow is rerouted during surgery. But that risk drops significantly in high-volume centers.
PCI’s biggest weakness is repeat revascularization. About 10-20% of stent patients need another procedure within five years. That’s because stents can re-narrow (in-stent restenosis) or new blockages can form nearby. CABG grafts, especially arterial ones, stay open longer. Arterial grafts have an 85-90% patency rate at 10 years. Vein grafts? Only 60-70%.
And here’s something most patients don’t think about: repeat procedures aren’t just inconvenient-they’re dangerous. Each time you go under the wire or the knife, your risk goes up.

The heart team: Why you need more than one doctor’s opinion
Guidelines now require a “heart team” approach. That means an interventional cardiologist and a cardiac surgeon sit down together-with you-to decide the best path. This isn’t bureaucracy. It’s science.
Studies show that hospitals with formal heart teams have lower mortality rates. At centers doing more than 400 PCIs or 200 CABGs a year, 30-day death rates are 1.8% for bypass. At low-volume hospitals? It’s 3.2%.
Don’t let a single doctor push you toward their specialty. Ask: “Did my case go through a heart team review?” If the answer is no, push for one. Your life depends on it.
What’s next? Hybrid procedures and better grafts
The future of revascularization isn’t just stents or bypass-it’s both. Hybrid procedures are emerging. For example, a surgeon might do a minimally invasive bypass to the left anterior descending artery (the most critical vessel), and a cardiologist places stents in other arteries. This combines the durability of surgery with the speed of stenting.
Also, surgeons are now using multiple arterial grafts instead of veins. Early data shows 10-year survival jumps from 74% to 82% with this approach. It’s not standard yet, but it’s coming.
And while bioresorbable stents (stents that dissolve) were pulled from the market due to safety issues, next-generation designs are in trials. They could one day offer the benefits of stenting without the long-term metal risk.
Bottom line: Match the treatment to your life
There’s no universal answer. But here’s how to think about it:
- If you’re young, diabetic, have complex blockages, or want the best long-term chance to avoid another surgery-choose CABG.
- If you’re older, have simple blockages, need to get back to work fast, or have high surgical risk-PCI may be the smarter first step.
- If your case is in the middle? Demand a heart team review. Don’t settle for a quick decision.
Both procedures save lives. But only one gives you a permanent fix for complex disease. Don’t choose based on fear of surgery. Choose based on data, your anatomy, and your future.
Is PCI safer than CABG?
PCI has lower immediate risks-less bleeding, shorter hospital stay, and lower stroke risk in the first 30 days. But CABG has lower long-term risks of heart attack and repeat procedures. Safety depends on the timeline. For short-term recovery, PCI wins. For long-term survival, especially with diabetes or complex disease, CABG is safer.
How long do stents and bypass grafts last?
Stents can last 5-10 years, but about 10-20% need another procedure within five years. Arterial bypass grafts-especially from the chest wall-have 85-90% patency at 10 years. Vein grafts last about 60-70%. The best long-term results come from using multiple arterial grafts, which are becoming more common.
Can I have PCI after CABG?
Yes. If a bypass graft becomes blocked or new blockages form in untreated arteries, PCI can be used to open them. Many patients who had CABG years ago later need stents for new or progressive disease. It’s not uncommon and is often very effective.
Why do some doctors prefer PCI over CABG?
PCI is less invasive, faster, and reimbursed less per procedure-so it’s more common. But many doctors also prefer it because patients recover quicker and are happier in the short term. The problem? Some don’t fully account for long-term outcomes, especially in high-risk patients. That’s why heart team reviews are critical.
What’s the recovery like after CABG?
Expect 5-7 days in the hospital. Full recovery takes 6-8 weeks. You’ll have chest soreness, fatigue, and possibly memory fog for a few weeks. Most people return to work by 6-8 weeks. By six months, 94% are back to normal activities. Long-term, most report better energy and no angina.
Does age matter in choosing PCI or CABG?
Age alone doesn’t decide it. A healthy 75-year-old with complex disease may benefit more from CABG than a 50-year-old with diabetes and poor health. What matters is biological age, frailty, and overall health-not just the number on your birth certificate. Heart teams assess fitness, not just age.