GI Medication Absorption Calculator
This calculator estimates how your gastrointestinal conditions and lifestyle factors affect medication absorption. Based on your inputs, it shows the estimated absorption percentage and explains key factors affecting your treatment.
Enter your information above to see your estimated absorption percentage.
Important Notes
This is a scientific estimate only. Actual absorption varies by individual physiology, disease activity, and other medications. Always follow your doctor's specific instructions.
Have you ever taken a pill exactly as directed, but still felt like it wasn’t working? For many people with digestive conditions, this isn’t just bad luck-it’s biology. Gastrointestinal medications face a hidden battle before they even reach your bloodstream. The gut isn’t just a tube for food; it’s a complex, dynamic barrier designed to keep things out, not let them in. And that’s exactly the problem when you need a drug to be absorbed.
Why Your Stomach and Intestines Fight Your Medication
The human digestive system is built to protect you. The stomach’s acid breaks down foreign substances. The small intestine has a thick mucus layer and tight junctions between cells that block unwanted molecules. Enzymes chew up proteins and other compounds. And then there’s the liver, which filters everything coming from the gut before it hits the rest of your body. This is called first-pass metabolism, and it can destroy up to 90% of some drugs before they ever get a chance to work. Most oral medications are absorbed in the small intestine, not the stomach. That’s because the small intestine has a massive surface area-roughly the size of a tennis court-thanks to tiny finger-like projections called villi and microvilli. But even here, not everything passes through easily. Drugs need to be small enough (under 500 Daltons), fat-soluble enough (log P >1), and stable enough to survive the journey. If your drug is too big, too watery, or too fragile, it won’t make it.Food, pH, and Timing: The Silent Saboteurs
You’ve probably heard to take some pills on an empty stomach. That’s not just a suggestion-it’s science. Fatty meals can slow down how fast your stomach empties by 2 to 4 hours. That delay can cut peak drug levels in your blood by 30% to 50%. For drugs like levothyroxine, which need precise, consistent absorption, even a small delay can throw off your entire hormone balance. The pH of your gut changes along its length. It’s acidic near the stomach (pH 4-5), then becomes more alkaline as you move toward the colon (up to pH 8). Many drugs dissolve better in certain pH ranges. If your gut’s pH shifts due to medication, disease, or even diet, your pill might not dissolve properly. A drug that works fine in a healthy person might sit in your intestine like a rock if your gut environment is altered.What Happens When Your Gut Is Sick?
If you have Crohn’s disease, ulcerative colitis, or short bowel syndrome, your body doesn’t just absorb nutrients poorly-it absorbs medications poorly too. In ulcerative colitis, patients often absorb 25% to 40% less of standard mesalamine doses than healthy people. That means the same pill that works for someone else might be completely ineffective for you. In short bowel syndrome, where parts of the intestine have been surgically removed, there’s simply not enough surface area left to absorb most drugs. Patients often need 2 to 3 times the normal dose of antibiotics, vitamins, or pain meds just to get the same effect. And even then, it’s not guaranteed. Even something as common as irritable bowel syndrome (IBS) can mess with absorption. Slowed or erratic gut movement delays how long a drug stays in the right spot to be absorbed. For extended-release pills, this can mean the drug gets pushed out before it has time to release. One pharmacist reported INR levels in IBD patients swinging from 1.5 to 4.5 on the same warfarin dose-dangerously unpredictable.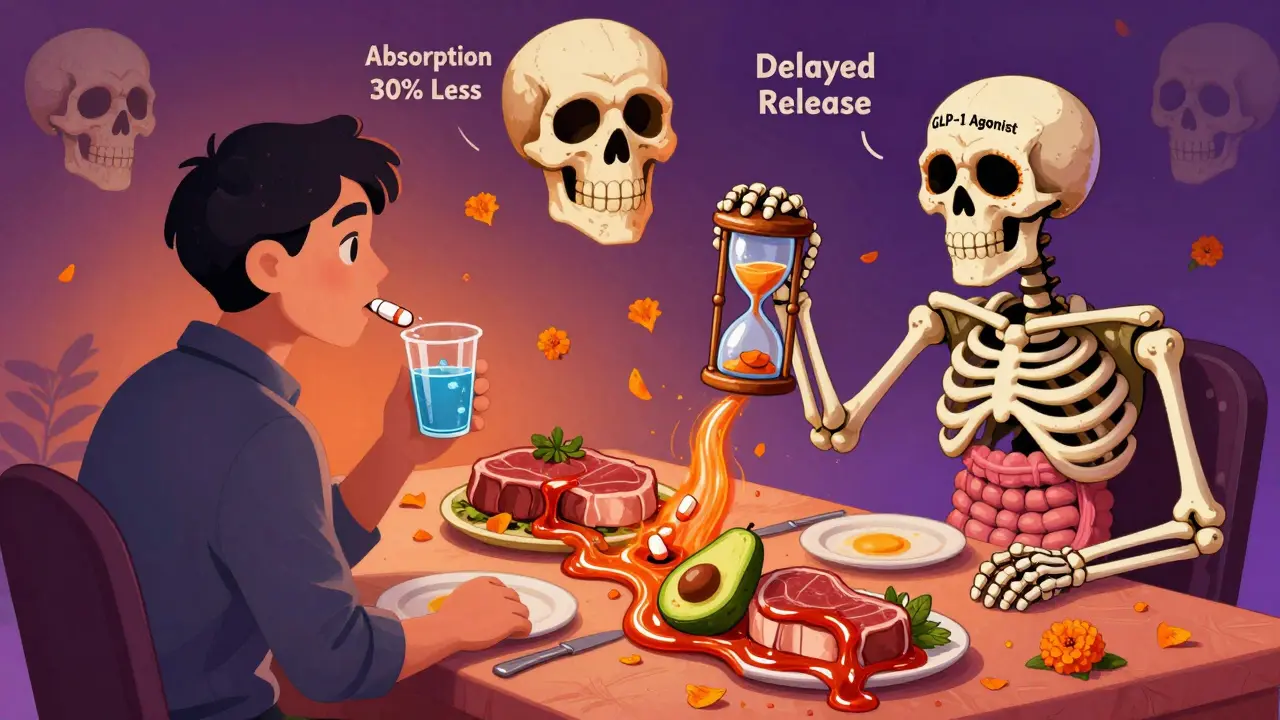
What About Newer Drugs Like Semaglutide?
GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) are changing how we treat diabetes and obesity. But they come with a side effect most people don’t talk about: they slow down gut motility. That’s good for blood sugar control, but bad for other medications. If you’re taking a blood thinner, seizure drug, or thyroid medicine, semaglutide can delay its absorption by 15% to 30%. That’s enough to cause underdosing-or, in rare cases, dangerous buildup if the drug eventually catches up. Doctors now have to ask: “Are you on any new weight-loss meds?” before prescribing anything else. This interaction isn’t listed on most drug labels. It’s learned through experience, not textbooks.Why Some Pills Just Don’t Work-Even If They’re the Right Dose
Not all pills are created equal. A tablet, capsule, or liquid might contain the same active ingredient, but how it’s made changes everything. Is it a plain powder? A salt form? A coated tablet? A nanoparticle? These choices affect how fast the drug dissolves, which is often the real bottleneck. For example, griseofulvin, an old antifungal, dissolves so slowly that its absorption depends almost entirely on how long it lingers in the gut. If your transit time is fast, it passes through before it can be absorbed. That’s why doctors tell you to take it with a fatty meal-it slows things down and helps the drug dissolve. Newer formulations are trying to fix this. Liposomes, polymeric nanoparticles, and lipid-based carriers can boost bioavailability by 1.5 to 3.5 times for drugs that normally struggle to be absorbed. Sodium caprate and chitosan can temporarily open the tight junctions between gut cells, letting bigger molecules sneak through. These aren’t magic-yet-but they’re being used in clinical trials for insulin, vaccines, and biologics that were once thought impossible to take orally.Why Your Doctor Might Not Know What’s Going Wrong
Most drug labels give no guidance for people with digestive diseases. The FDA-approved instructions for a common antibiotic might say “take with food,” but won’t tell you what to do if you have Crohn’s and can’t digest fats. Pharmacists and gastroenterologists often have to piece together clues from scattered studies, patient reports, and trial-and-error. One patient on the Crohn’s & Colitis Foundation forum wrote: “My Remicade levels fluctuate wildly-sometimes therapeutic, sometimes undetectable-even with consistent dosing.” That’s not a failure of the drug. That’s a failure of the system. The body’s absorption is unpredictable, and we still don’t have good tools to measure it in real time.
What Can You Do?
If you’re on GI meds and they’re not working:- Take them exactly as directed-on an empty stomach, with water, at the same time every day.
- Track your symptoms and drug timing. Note if your absorption seems worse after meals, during flare-ups, or after starting a new medication.
- Ask your doctor about blood level monitoring (like for warfarin or immunosuppressants) if you have a chronic condition.
- Request specialized formulations: liquid, chewable, or extended-release versions may work better than standard tablets.
- Be upfront about all medications, supplements, and weight-loss drugs you’re taking. GLP-1 agonists can interfere with many others.
The Future: Personalized Gut Medicine
Scientists are now building digital models of individual guts using data from pH sensors, motility trackers, and genetic profiles. Early trials (like NCT04567890) are testing smart capsules that measure gut conditions in real time and signal when to release a drug for maximum absorption. Imagine a pill that waits until your gut is in the perfect state to release its contents-no more guesswork. The global market for absorption enhancers is projected to hit $2.8 billion by 2027. That’s because we’re moving beyond one-size-fits-all pills. The future of GI meds isn’t just stronger drugs-it’s smarter delivery.Bottom Line
Gastrointestinal medications don’t fail because you’re not trying hard enough. They fail because the gut is a fortress, and most drugs weren’t built to break through. Whether you’re dealing with IBD, IBS, surgery, or just a slow digestive system, your body’s absorption capacity matters more than the dose on the bottle. If your meds aren’t working, it’s not your fault. It’s a system problem-and the fix is coming, but it’s not here yet. In the meantime, knowledge is your best tool.Why do some GI medications work for some people but not others?
It comes down to individual differences in gut physiology. Factors like disease severity, transit time, pH levels, mucus thickness, and even gut bacteria vary widely between people. Two patients with the same diagnosis can absorb the same drug at completely different rates. A drug that works perfectly in a healthy gut might be useless in an inflamed or shortened intestine. That’s why personalized dosing and monitoring are becoming essential.
Can food really make a medication ineffective?
Yes, especially with drugs that need fast, consistent absorption. Fatty meals delay gastric emptying, which can reduce peak drug levels by 30-50%. For medications like levothyroxine, antibiotics, or certain antifungals, this delay can drop effectiveness below therapeutic levels. On the flip side, some drugs (like griseofulvin) need fat to dissolve properly. The key is following exact instructions-not guessing.
Why don’t drug labels warn about absorption issues in IBD or IBS?
Most drug labels are based on trials in healthy adults. Only about 15-20% of oral medications have specific dosing guidance for patients with inflammatory bowel disease or other GI conditions. This gap exists because testing drugs in sick populations is expensive and complex. Doctors and pharmacists have to rely on clinical experience and specialty guidelines from groups like the American Gastroenterological Association to fill in the blanks.
Are there better forms of GI medications than pills?
Yes. For children, elderly patients, or those with swallowing issues, liquid or chewable forms are often more reliable. In IBD, delayed-release or targeted-release formulations (like Asacol HD) are designed to release drug in the colon-but they can fail if inflammation is too severe. For patients with short bowel syndrome, liquid suspensions or compounded doses are often needed. Newer nanoparticle and lipid-based formulations are also showing promise for better absorption.
How do GLP-1 drugs like Ozempic affect other medications?
GLP-1 agonists slow down how fast food and drugs move through the gut. This can delay absorption of other oral medications by 15-30%, especially those with narrow therapeutic windows like warfarin, levothyroxine, or seizure drugs. This delay can lead to underdosing, or later spikes in drug levels that cause side effects. Always tell your doctor if you start or stop a GLP-1 medication-they may need to adjust your other prescriptions.
Is there a test to see how well my body absorbs medications?
For some drugs, yes. Blood level monitoring (therapeutic drug monitoring) is used for medications like warfarin, cyclosporine, and certain antibiotics. If your levels are consistently low despite taking the right dose, it could mean poor absorption. Researchers are also developing smart capsules with sensors to measure pH, pressure, and transit time in real time-still experimental, but promising for the future.








