Antioxidant Supplement Comparison Tool
Select Antioxidants to Compare
Choose which supplements you'd like to view side-by-side
Antioxidant Comparison
Recommended Supplement Bundle
Most clinicians recommend combining multiple antioxidants for best results:
Try starting with Vitamin C + Vitamin E + NAC for a balanced approach that targets both water-soluble and fat-soluble oxidative damage.
Remember: Always take fat-soluble antioxidants (Vitamin E, Selenium) with meals containing healthy fats for better absorption.
Important Safety Considerations
Living with chronic pancreatitis feels like constantly walking a tightrope between pain, digestion problems, and the fear of long‑term damage. One piece of the puzzle that’s gaining attention is antioxidant supplementation. By targeting the hidden enemy of oxidative stress, these nutrients may ease inflammation and protect pancreatic tissue.
Chronic pancreatitis and oxidative stress
When doctors diagnose Chronic Pancreatitis as a persistent inflammatory condition of the pancreas that leads to irreversible damage and loss of exocrine function, they are looking at a disease driven by repeated injury. Alcohol abuse, gallstones, genetic mutations, and autoimmune disorders can all trigger repeated attacks. Each flare releases reactive oxygen species (ROS) that overwhelm the pancreas’s natural antioxidant defenses.
The imbalance between ROS and antioxidants is called Oxidative Stress, a state where free radicals damage proteins, lipids, and DNA, accelerating tissue fibrosis and pain. Studies from the past decade show that patients with chronic pancreatitis have significantly lower serum levels of key antioxidants, suggesting that replenishing these defenses could slow disease progression.
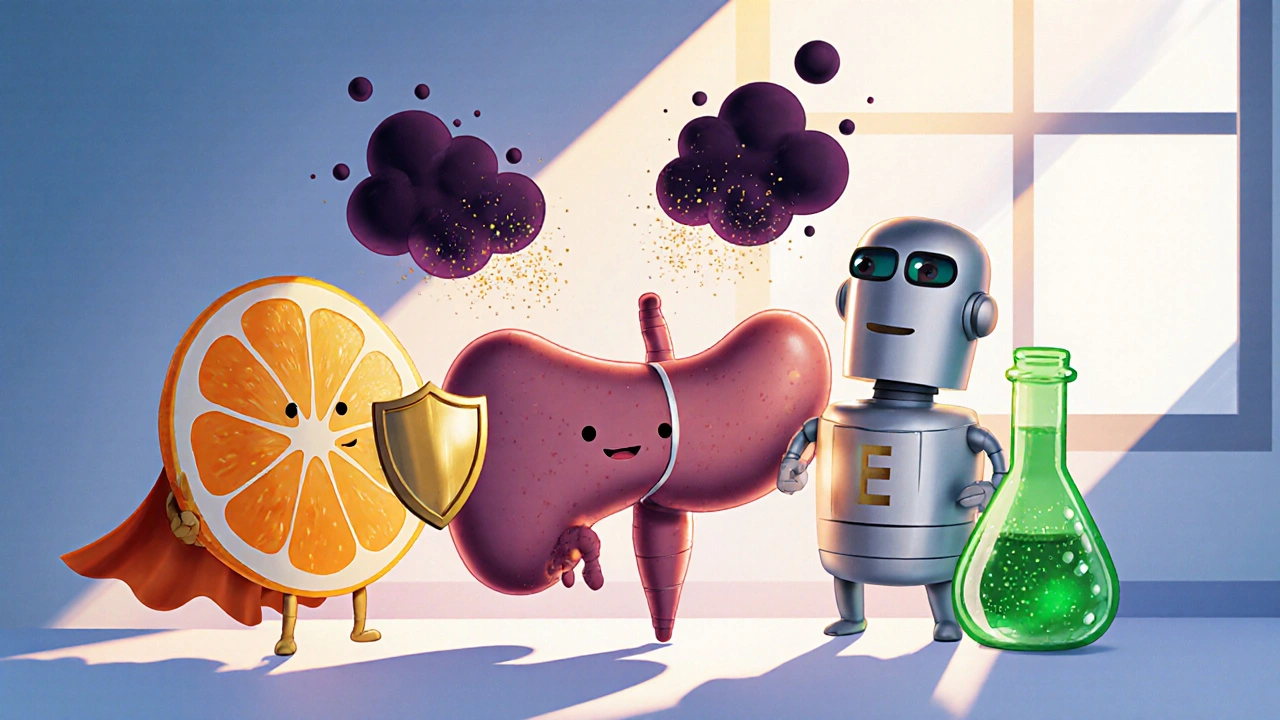
Why antioxidants matter in pancreatic care
Antioxidants act as molecular “sponges,” neutralizing free radicals before they can wreak havoc. In the pancreas, this translates into reduced inflammation, less fibrosis, and better preservation of the cells that produce digestive enzymes. Clinical trials involving vitamin C, vitamin E, selenium, and N‑acetylcysteine (NAC) have reported modest improvements in pain scores and quality of life when added to standard therapy.
It’s not a magic bullet, but when paired with pancreatic enzyme replacement therapy (PERT) and lifestyle changes, antioxidants create a multi‑layered defense that addresses both symptoms and underlying cellular damage.
Common antioxidants used for chronic pancreatitis
Below is a snapshot of the most researched supplements. Doses listed are typical therapeutic ranges; individual needs may vary.
| Antioxidant | Primary action | Typical dose | Evidence level | Common side effects |
|---|---|---|---|---|
| Vitamin C, a water‑soluble antioxidant that scavenges ROS and regenerates other vitamins | Neutralizes free radicals, supports collagen synthesis | 500‑1000mg daily | Moderate (several small RCTs) | GI upset, kidney stones at very high doses |
| Vitamin E, a fat‑soluble tocopherol that protects cell membranes from lipid peroxidation | Stabilizes membranes, modulates inflammation | 400‑800IU daily | Moderate (meta‑analysis of 5 trials) | Bleeding risk in anticoagulated patients |
| Selenium, a trace mineral essential for glutathione peroxidase activity | Boosts endogenous antioxidant enzymes | 100‑200µg daily | Low (single pilot study) | Hair loss, nail brittleness at excess levels |
| N‑acetylcysteine (NAC), a precursor to glutathione that directly scavenges ROS | Replenishes intracellular glutathione | 600‑1200mg twice daily | Moderate (controlled trials show pain reduction) | Bronchospasm, nausea |
| Glutathione, the master intracellular antioxidant that detoxifies peroxides | Detoxifies free radicals, supports immune function | 250‑500mg daily (liposomal form preferred) | Low (mostly animal studies) | Rare, mild GI discomfort |
Choosing the right supplement and dosing strategy
Start by getting baseline labs: serum vitamin C, vitamin E, selenium, and a glutathione‑peroxidase activity test if available. If any value is low, that antioxidant becomes the first target.
Most clinicians recommend a “bundle” approach: combine a water‑soluble antioxidant (vitamin C) with a fat‑soluble one (vitamin E) and a glutathione precursor (NAC). This covers multiple pathways of oxidative damage.
Timing matters. Take vitamin C and NAC on an empty stomach for better absorption, while vitamin E and selenium are best with a meal that contains some fat.
Re‑evaluate every three months. Adjust doses if pain improves or if side effects appear. Remember that more isn’t always better-excess vitamin E can interfere with blood clotting, and too much selenium becomes toxic.
Safety, drug interactions, and monitoring
Antioxidants are generally safe, but they do interact with certain medications. Vitamin E can potentiate the effect of warfarin and other anticoagulants, raising bleeding risk. High‑dose vitamin C may increase oxalate formation, which is a concern for patients prone to kidney stones.
Patients on chemotherapy or radiation should discuss antioxidant use with their oncologist, as some agents rely on oxidative mechanisms to kill cancer cells.
Monitoring plan:
- Every 3months: pain diary, weight, and digestive symptom log.
- Every 6months: serum antioxidant panel and liver function tests.
- Immediately: report any unusual bruising, dark urine, or severe abdominal pain.
If any adverse reaction occurs, reduce the dose or pause the supplement for two weeks and reassess.

Integrating antioxidants with standard pancreatic therapy
Standard care for chronic pancreatitis includes pancreatic enzyme replacement therapy (PERT), pain management, dietary modifications, and abstinence from alcohol and smoking. Antioxidants should sit alongside, not replace, these pillars.
For example, a typical regimen might look like:
- Take prescribed PERT capsules with each main meal and snack.
- Consume a low‑fat, high‑protein diet with small, frequent meals.
- Start antioxidant bundle: 500mg vitamin C, 400IU vitamin E, 100µg selenium, and 600mg NAC taken as split doses.
- Track pain scores and stool consistency daily.
- Review labs and symptoms with the gastroenterologist every 3months.
This integrative approach gives the pancreas the enzymes it needs while shielding its cells from oxidative injury.
Practical checklist for patients
- Confirm diagnosis of chronic pancreatitis with imaging and labs.
- Ask your doctor for baseline antioxidant levels.
- Choose high‑quality supplements (third‑party tested, no unnecessary additives).
- Start with low doses; increase gradually based on tolerance.
- Take fat‑soluble antioxidants with meals that contain healthy fats.
- Maintain a symptom journal - pain, bloating, stool changes.
- Schedule lab checks every six months.
- Discuss any new meds or herbal products with your healthcare team.
Frequently Asked Questions
Can antioxidant supplements cure chronic pancreatitis?
No. Antioxidants help reduce oxidative damage and may lower pain, but they do not reverse already scarred pancreatic tissue. They work best as part of a broader treatment plan.
How long should I stay on antioxidant therapy?
Most clinicians recommend at least six months of continuous use, followed by a reassessment of symptoms and lab values. Some patients stay on low‑dose maintenance indefinitely.
Are natural food sources enough, or do I need pills?
A diet rich in fruits, vegetables, nuts, and seeds provides antioxidants, but therapeutic doses often exceed what food alone can deliver. Supplements ensure you reach the levels studied in clinical trials.
Will antioxidants interfere with my pain medication?
Generally they do not, but high doses of vitamin E can increase bleeding risk if you’re on opioids that contain acetaminophen or on anticoagulants. Always check with your prescriber.
Is there any risk of taking too many antioxidants?
Yes. Over‑supplementation can lead to toxicity, such as selenium poisoning or vitamin E‑related bleeding. Stick to recommended therapeutic ranges and have labs checked regularly.