Every year, thousands of people end up in emergency rooms because they didn’t know drinking alcohol with their prescription meds could kill them. It’s not just about getting drunk. It’s about your body reacting in ways you can’t predict - slower breathing, crashing blood pressure, liver failure, or even stopping breathing entirely. This isn’t rare. In 2022 alone, alcohol and prescription drugs were linked to over 2,300 overdose deaths in the U.S. And most of these cases could have been avoided.
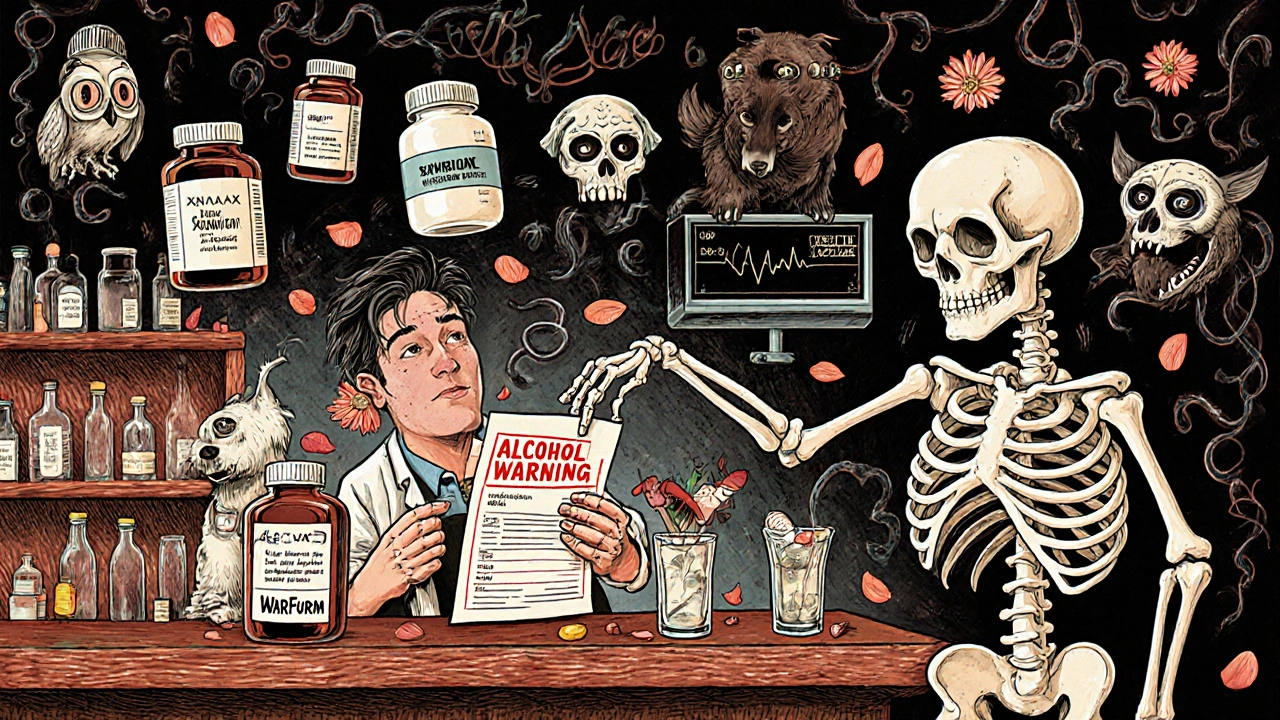
How Alcohol Changes How Your Meds Work
Your body treats alcohol and many medications the same way: it tries to break them down in the liver using the same enzyme system, called cytochrome P450. When you drink, it messes with this process. Sometimes alcohol makes your meds work too well - building up to toxic levels. Other times, it makes them useless.For example, if you take warfarin (a blood thinner) and have even one drink, alcohol can slow down how fast your liver clears it. That means your blood doesn’t clot properly, and you could bleed internally without knowing it. One study found alcohol can increase warfarin levels in the blood by up to 35%.
On the flip side, if you drink regularly - say, a few drinks most days - your liver starts making more enzymes to handle the alcohol. That means it also breaks down meds like propranolol (used for high blood pressure) faster. In some cases, the drug’s effect drops by half. You think it’s working, but it’s not. Your blood pressure stays high, and you’re at risk for a heart attack or stroke.
High-Risk Combinations: The Deadliest Mixes
Some meds don’t just interact - they team up with alcohol to create a perfect storm. The most dangerous are opioids and benzodiazepines.Opioids like oxycodone, hydrocodone, and morphine already slow your breathing. Alcohol does the same. Together, they multiply that effect by six times. Even one drink with a normal dose of an opioid can turn a safe prescription into a fatal one. The CDC says alcohol-opioid combinations cause 26% of all prescription drug overdose deaths. Blood alcohol levels as low as 0.02% - the amount from one beer - double your risk of a fatal crash if you’re on opioids.
Benzodiazepines - like Xanax, Valium, or lorazepam - are prescribed for anxiety or sleep. They make you drowsy. Alcohol does too. Combine them, and you’re not just sleepy. You’re dangerously sedated. Research shows the sedation effect increases by 400% compared to either substance alone. Older adults are especially vulnerable. In nursing homes, 78% of falls linked to these drugs happened in people who drank within six hours.
Other Dangerous Pairings You Might Not Expect
It’s not just the heavy-hitters. Everyday meds can turn risky with alcohol too.Acetaminophen (Tylenol) is the most common painkiller in American homes. But when you drink, even moderately, your liver turns acetaminophen into a toxic chemical. One in 200 regular drinkers who take acetaminophen develop acute liver failure. That’s not a typo - it’s a real, documented risk. The FDA issued a safety warning in 2020 after seeing dozens of cases linked to this combo.
NSAIDs like ibuprofen or naproxen are fine for occasional use. But if you drink three or more drinks a day, your risk of stomach bleeding goes up by 300%. That’s because alcohol irritates your stomach lining, and NSAIDs weaken your body’s ability to protect itself. You might not feel pain until it’s too late.
Antidepressants like SSRIs (Prozac, Zoloft) don’t cause fatal interactions, but they make you drowsy. One study found 35% of people over 65 who drank even one or two drinks a day while on SSRIs felt so tired they nearly fell. That’s a huge fall risk. And falls in older adults often lead to broken hips, long hospital stays, or worse.
Antibiotics like metronidazole or tinidazole can cause violent reactions - nausea, vomiting, rapid heartbeat - when mixed with alcohol. Even amoxicillin, which is usually safe, can cause liver stress if you’re a heavy drinker. Isoniazid, used for tuberculosis, causes liver damage in 15% of users who drink.
Who’s Most at Risk?
It’s not just about how much you drink. Your body matters too.Aging: After 65, your liver processes alcohol slower. Your body has less water, so alcohol stays in your system longer. Older adults are 3.2 times more likely to have severe interactions. That’s why the American Geriatrics Society lists 15 alcohol-interacting drugs as “potentially inappropriate” for seniors.
Gender: Women are more vulnerable. On average, they have less body water and more fat. That means alcohol concentrates more in their blood. Even the same drink affects women 20% more than men.
Liver disease: If you have cirrhosis or fatty liver, your liver can’t handle anything extra. Acetaminophen becomes deadly at much lower doses. Alcohol can trigger sudden liver failure even in people who never had a problem before.
Why So Many People Don’t Know
You’d think doctors and pharmacists would warn you. But they often don’t.A 2023 review of 12,450 patient reviews on Healthgrades found 68% of people prescribed benzodiazepines were never told not to drink. One Reddit user shared: “Prescribed oxycodone after wisdom teeth surgery. No warning about alcohol. Had two beers. Couldn’t breathe for 20 minutes.”
Even when warnings exist, they’re inconsistent. Only 38% of benzodiazepine prescriptions have clear alcohol warnings on the label, according to an FDA audit. And 43% of primary care doctors couldn’t name all the high-risk meds in a 2023 test.
Patients themselves are confused. A WebMD survey of 5,842 adults found 57% believed “one drink is safe with most medications.” Thirty-two percent thought only hard liquor was dangerous. That’s wrong. Beer, wine, and liquor all contain alcohol - and they all interact.
What You Can Do - Right Now
You don’t need to be an expert to stay safe. Here’s how to protect yourself:- Check the label. Look for “Do not drink alcohol” or “May cause drowsiness” - those are red flags.
- Ask your pharmacist. They’re trained to catch these interactions. Use the 4-question screening tool: “Do you drink alcohol? How often? How much? Are you taking any other meds?”
- Use the NIAAA Alcohol Medication Check app. It scans over 2,300 medications and tells you if alcohol is risky with yours.
- When in doubt, skip it. If your med has any warning - even vague ones like “may cause dizziness” - avoid alcohol until you’ve talked to a professional.
One patient in Calgary wrote on Google Reviews: “My Walgreens pharmacist refused to fill my lorazepam prescription when I admitted I drank daily. Said I could die. I didn’t believe her until I read the warning online. She saved my life.”
What’s Changing - And What’s Coming
Hospitals are catching on. The VA system now screens every patient for alcohol use before filling prescriptions. 73% of U.S. hospitals use real-time systems that flag dangerous combos as soon as a doctor writes a script. These systems have cut interaction-related hospitalizations by 28%.The FDA is requiring clearer labels. The 2022 Alcohol-Drug Interaction Labeling Act means 147 million prescriptions a year must now carry bold “ALCOHOL WARNING” notices.
Future tools are even smarter. Epic Systems rolled out AI in 2024 that analyzes 200+ patient factors - age, liver enzymes, drinking habits, genetics - to predict your personal risk level. It’s 89% accurate.
But technology won’t fix everything. A 2023 study found only 28% of high-risk patients stop drinking, even after being warned. The real challenge isn’t knowledge - it’s behavior.
Final Word: It’s Not Worth the Risk
You might think, “I only have one glass of wine.” Or, “I take my pill at night, I drink at lunch.” But alcohol doesn’t wait. It’s still in your system 12 hours later. And your meds? They’re working all day.There’s no safe amount of alcohol with opioids or benzodiazepines. There’s no safe amount with acetaminophen if you drink regularly. And if you’re over 65? Even one drink can tip you into danger.
The data doesn’t lie. The deaths are real. The warnings are there. You don’t need to give up everything - but if you’re on a prescription, you need to know if alcohol is part of the deal. Because sometimes, the thing that’s supposed to help you - your medicine - becomes the thing that kills you, if you drink with it.
Can I have one drink with my prescription medication?
It depends on the medication. With opioids, benzodiazepines, or acetaminophen, even one drink can be dangerous. With some antibiotics or blood pressure meds, one drink might be okay - but only if your doctor says so. Never assume. Always check.
Do all medications have alcohol warnings on the label?
No. Only 65% of high-risk prescriptions include clear alcohol warnings. Many labels use vague language like “may cause drowsiness” or don’t mention alcohol at all. That’s why you can’t rely on the label alone - talk to your pharmacist.
Is beer less dangerous than liquor with meds?
No. A 12-ounce beer, a 5-ounce glass of wine, and a 1.5-ounce shot of liquor all contain the same amount of alcohol. The type doesn’t matter - the alcohol does. Any form of alcohol can interact with your meds.
I’m over 65. Should I stop drinking completely if I take meds?
For high-risk meds like sleep aids, anxiety drugs, or painkillers - yes. For others, talk to your doctor. But given that older adults process alcohol slower and are more sensitive to side effects, most experts recommend avoiding alcohol entirely if you’re on multiple prescriptions.
Can my pharmacist refuse to fill my prescription if I drink?
Yes. Pharmacists are trained to prevent harm. If they believe alcohol could cause a dangerous interaction, they can delay or refuse to fill the prescription until you speak with your doctor. This is not unusual - and it’s often lifesaving.