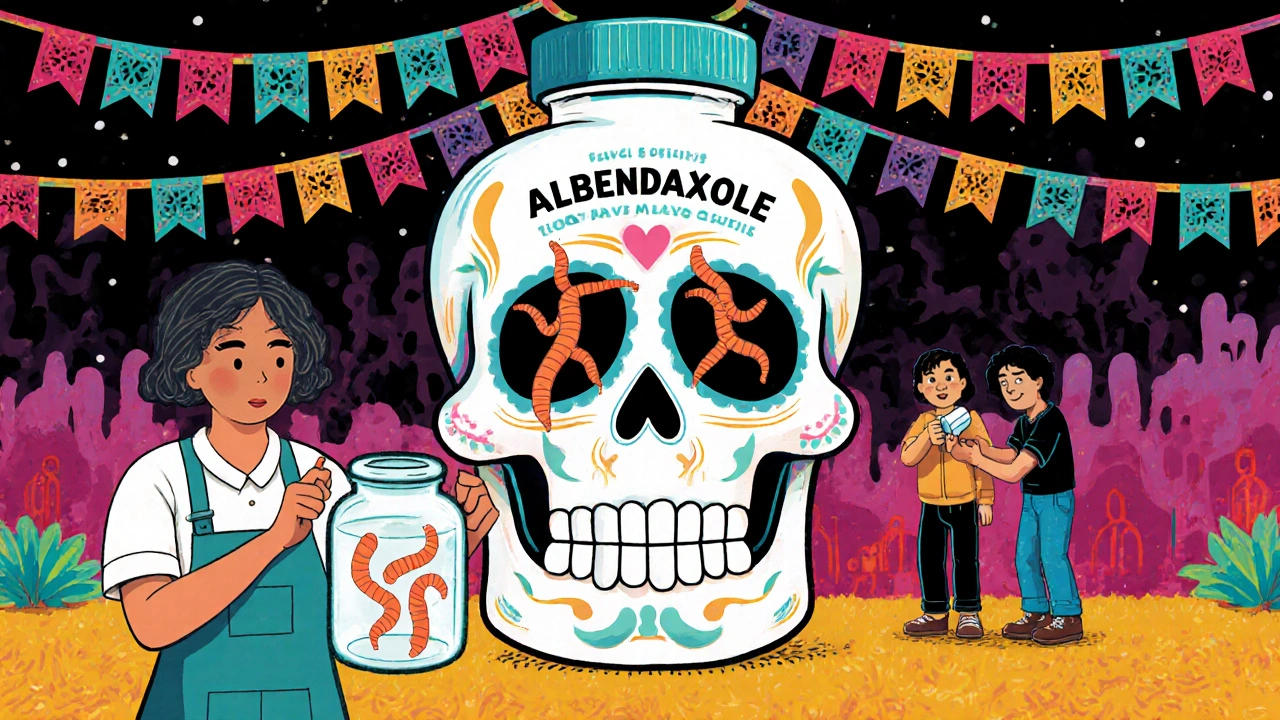
Albendazole used to be the go-to pill for worm infections. It worked on roundworms, hookworms, whipworms, and even tapeworms. But now, in many places, it doesn’t work like it used to. People take the full dose, follow the instructions, and still the worms come back. This isn’t just bad luck-it’s albendazole resistance, and it’s growing fast.
What Albendazole Resistance Really Means
Albendazole resistance isn’t the drug getting weaker. It’s the parasites adapting. These tiny worms have been exposed to albendazole for decades. In places where mass drug administration programs run yearly-like in parts of Africa, South Asia, and Latin America-the worms that survive the treatment pass on their resistant genes. Over time, the population shifts. The worms that used to die in hours now live through the dose.
Studies from Nepal and Ethiopia show that in some villages, more than 40% of whipworm infections no longer respond to standard albendazole doses. In one 2023 trial in Uganda, after three rounds of treatment, egg reduction rates dropped from 95% to just 58%. That’s not a small drop. That’s a system breaking down.
Why Resistance Is Spreading So Fast
There are three big reasons albendazole resistance is climbing.
- Overuse in humans: In high-risk areas, entire communities get albendazole every year-even people who don’t have worms. This creates constant pressure on parasites to evolve.
- Underdosing: Some people take half a pill because they’re scared of side effects. Others use leftover medicine from past infections. Both leave just enough drug in the system to kill the weak worms but let the strong ones survive.
- Use in livestock: Albendazole is widely used in cattle, sheep, and goats. In many countries, the same drug is given to animals and humans. Resistant worms from farms can spread to people through contaminated soil or water.
It’s not just one mistake. It’s a perfect storm of good intentions and poor execution. Mass deworming programs save lives-but without monitoring, they’re also breeding superworms.
How Scientists Know It’s Resistance, Not Poor Absorption
Some say, "Maybe the drug isn’t being absorbed properly." But that’s not it. Researchers tested this by measuring drug levels in blood after dosing. In resistant cases, the albendazole concentration in the blood was normal. The drug reached the worms. The worms just didn’t die.
Lab tests show resistant worms have changes in their cells. They pump the drug out faster using special proteins called efflux pumps. Some have mutations in a gene called β-tubulin, which is albendazole’s target. The drug can’t bind properly anymore. It’s like the lock changed shape, and the key no longer fits.
What Works When Albendazole Fails
If albendazole isn’t working, you need alternatives. But not all options are equal.
- Mebendazole: Often used as a substitute, but it’s in the same drug class. If albendazole failed, mebendazole likely will too.
- Praziquantel: Great for tapeworms and flukes, but useless against roundworms and hookworms.
- Ivermectin: Works well against some soil-transmitted worms, especially in combination with albendazole. In Ghana, adding ivermectin to albendazole boosted cure rates from 52% to 89% in whipworm cases.
- Thiabendazole: Older drug, rarely used now. Toxic side effects make it a last resort.
The most promising combo right now is albendazole + ivermectin. It’s not a silver bullet, but in trials across Southeast Asia, it cut treatment failure rates by more than half. It’s not approved everywhere yet, but WHO is reviewing it for wider use.
Real-World Solutions: What Works on the Ground
Fixing this isn’t just about new drugs. It’s about changing how we use the ones we have.
- Test before you treat: Instead of giving albendazole to everyone, test stool samples first. Only treat those with confirmed infections. This reduces drug pressure.
- Use combination therapy: Start with albendazole + ivermectin in areas with known resistance. Don’t wait until it fails completely.
- Rotate drugs: In livestock, switching between different anthelmintic classes every year slows resistance. We need the same strategy for humans.
- Improve sanitation: No drug works if people keep stepping in contaminated soil. Clean water, toilets, and shoe-wearing reduce reinfection rates by up to 70%.
- Track resistance: Health programs need simple, cheap tests to monitor worm responses. A $2 stool test done once a year can prevent a full-blown crisis.
In Vietnam, a pilot program in three provinces started testing for resistance and switching to combination therapy. Within two years, treatment success rates jumped from 55% to 87%. It wasn’t expensive. It just required better planning.

What You Can Do Right Now
If you’re a patient: Don’t take leftover albendazole. Don’t split pills. If you’ve been treated and still feel symptoms, go back. Ask for a stool test. Don’t assume it’s the same worm.
If you’re a caregiver or community health worker: Record treatment outcomes. Note who comes back with symptoms. Push for better diagnostics. Don’t just hand out pills-track results.
If you’re in a country with livestock: Avoid using human-grade albendazole on animals. Use vet-approved alternatives. Don’t let farm worms become human problems.
The Bigger Picture
Albendazole resistance isn’t just a parasite problem. It’s a warning. We’ve seen this with antibiotics. We thought we’d won. We didn’t. We kept using the same tools the same way. Now we’re paying the price.
Worms don’t care about borders. They don’t care about wealth. They just survive. And if we keep treating them like they’re easy to kill, they’ll keep outsmarting us.
The solution isn’t waiting for a new drug. It’s changing how we use the ones we have. Better testing. Better combinations. Better habits. It’s not glamorous. But it works.
Frequently Asked Questions
Can albendazole resistance be reversed?
Not easily, and not quickly. Once resistant worms dominate a population, stopping the drug for years might reduce their numbers-but they don’t disappear. The genes stay in the population. The best approach is to prevent resistance from spreading in the first place by using combination therapy and reducing unnecessary use.
Is albendazole resistance common in North America?
No, not yet. Albendazole resistance is mostly a problem in tropical and subtropical regions with high rates of soil-transmitted worms and frequent mass drug administration. In Canada and the U.S., infections are rare and usually travel-related. Treatment is targeted, not mass, so resistance hasn’t taken hold.
Can I take albendazole and ivermectin together?
Yes, but only under medical supervision. The combination is more effective than either drug alone, especially in areas with known resistance. However, both drugs can cause dizziness or nausea. A doctor should confirm the diagnosis and dosage before combining them.
Why not just make a new drug?
New anthelmintic drugs are expensive and slow to develop. The last major one, oxfendazole, was approved for animals in the 1990s. Human trials take over a decade and cost hundreds of millions. Meanwhile, resistance is spreading now. We can’t wait. The smart move is using what we have better-not waiting for something new.
Are there natural remedies that work against resistant worms?
No. Claims about pumpkin seeds, garlic, or wormwood killing resistant worms are not backed by science. In some cases, they delay proper treatment. If you suspect a worm infection, get a stool test and follow medical advice. Natural remedies don’t stop resistance-they make it worse.