When a panic attack hits, time doesn’t slow down-it vanishes. Your heart pounds like it’s trying to escape your chest. Your breath turns shallow. Your thoughts spiral: Is this a heart attack? Am I dying? I can’t control this. In those moments, logic disappears. But you don’t have to wait for the storm to pass. There’s a plan. And it’s not complicated. It’s simple. And it works.
Why a Panic Attack Action Plan Matters
Panic attacks aren’t just "bad anxiety." They’re full-body emergencies triggered by your nervous system going into overdrive. The National Institute of Mental Health says about 4.7% of U.S. adults will have at least one in their lifetime. That’s nearly 1 in 20 people. Most don’t know what’s happening. They think they’re dying. They call 911. They end up in the ER. And then they go home, scared it’ll happen again. The good news? Panic attacks are treatable. And the most effective way to stop them isn’t waiting for a doctor’s appointment. It’s having a personal action plan-something you can use the second you feel it coming. Research from Harvard Health Publishing and the American Psychological Association shows that structured plans combining breathing, grounding, and medication (when needed) reduce panic frequency by up to 70%. But only if you practice them when you’re calm.Step One: Breathing to Reset Your Nervous System
When you panic, you hyperventilate. You breathe fast and shallow, blowing out too much carbon dioxide. That drops the CO2 levels in your blood. And that’s what makes your fingers tingle, your vision blur, your chest tighten. It’s not a heart attack. It’s your body misreading the signals. The fix? Slow, controlled breathing. Not just any breathing. You need to retrain your body. Start with the 2-2-6 technique:- Inhale through your nose for 2 seconds
- Hold your breath for 2 seconds
- Exhale slowly through your nose for 6 seconds
- Pause for 1 second before repeating
Step Two: Grounding to Pull Yourself Back to Reality
Panic attacks pull you into your head. Into the fear. Into the worst-case scenarios. Grounding is the opposite. It’s about reconnecting with the world outside your mind. The most powerful tool? Recognizing what’s happening. The moment you feel the rush, say to yourself: This is a panic attack. It’s not dangerous. It will pass. That simple label reduces symptoms by 32% within 90 seconds, according to the Anxiety and Depression Association of America. Then, use your senses. Try the 5-4-3-2-1 method:- Look around. Name 5 things you can see.
- Touch four things. Feel their texture. A chair. Your jeans. Your phone.
- Listen. Name 3 sounds.
- Smell. What can you smell? Coffee? Soap? Fresh air?
- Taste. What’s in your mouth? Toothpaste? Water?

Step Three: Medication-When and How to Use It
Medication isn’t a magic fix. But it can be a bridge. There are two types used for panic attacks: SSRIs (like sertraline or paroxetine) are daily pills. They don’t work right away. It takes 8 to 12 weeks. But they reduce panic frequency by 60-70%. They’re not addictive. They’re not a quick fix. They’re a long-term reset for your brain chemistry. The Anxiety and Depression Association of America reports that 79% of people who stick with SSRIs for six months say the benefits outweigh the initial side effects-nausea, sleep trouble, fatigue. Benzodiazepines (like alprazolam or clonazepam) work fast. In 15 to 30 minutes, they can cut panic symptoms by 75%. That’s why some people keep them on hand. But here’s the catch: they’re dangerous if used too often. The FDA says 23% of people who take them daily for more than four weeks develop tolerance. That means they need more to get the same effect. And stopping suddenly can cause seizures. The rule? Use benzodiazepines only for emergencies. One pill, once in a while. Never daily. Never as your only tool. They’re a safety net, not a crutch. Research from Kaiser Permanente shows that people who combine medication with breathing and grounding techniques have a 68% success rate in long-term recovery. Those who rely only on pills? Only 42%.How to Build Your Own Action Plan
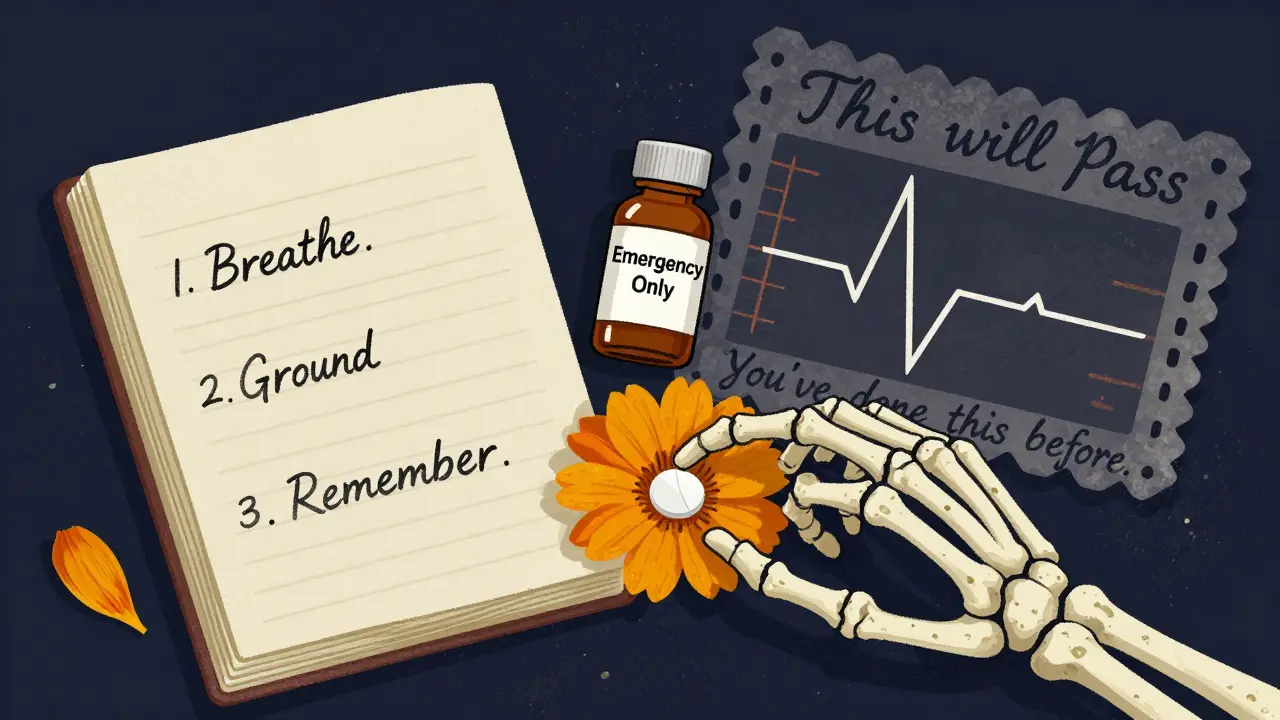
You don’t need a therapist to make this work. But you do need structure. Start with this 3-step system:- Write it down. On paper. Or in your phone. One page. Three sections: Breathing, Grounding, Medication.
- Practice daily. Even when you’re calm. Do 5 minutes of breathing every morning. Use grounding techniques while waiting in line. Make it routine.
- Prepare for panic. Put your plan where you’ll see it. On your bathroom mirror. In your wallet. Set a phone reminder: “Breathe. Ground. Remember-you’re safe.”
Common Mistakes (And How to Avoid Them)
Most people fail not because the plan doesn’t work. They fail because they do it wrong.- Mistake: Only using techniques during panic. Solution: Practice when you’re calm. Your brain needs muscle memory.
- Mistake: Relying on benzodiazepines too much. Solution: Keep them locked away. Use them only if you can’t breathe or ground yourself.
- Mistake: Waiting for perfection. Solution: Even one deep breath helps. One grounding thought counts. Progress isn’t linear.
- Mistake: Feeling ashamed. Solution: Panic doesn’t mean weakness. It means your nervous system got stuck. You’re not broken. You’re learning.
What Helps Beyond the Plan
Your action plan is the core. But support matters.- Apps: The “Panic Relief” app from UC San Francisco has guided breathing and grounding exercises. 4.3 stars from over 1,800 users.
- Webinars: The Anxiety and Depression Association of America offers free online sessions. 42% of participants say they learned more in one hour than in months of therapy.
- Wearables: Some people use heart rate monitors to catch early signs of panic-like a spike in pulse before the thoughts kick in. That gives you 10 minutes to breathe before it escalates.
When to See a Professional
You can do a lot on your own. But if you’re having more than two panic attacks a week, avoiding places because you fear an attack, or feeling depressed because of it-talk to someone. Cognitive behavioral therapy (CBT) is the gold standard. It’s not just talking. It’s training. You learn to challenge catastrophic thoughts. You face fears slowly. You rebuild confidence. And it works as well as medication-with no side effects. The American Psychological Association gives CBT the highest rating for panic disorder. And the best part? You can start with a self-guided workbook like Mastery of Your Anxiety and Panic (2021 edition). It’s structured. It’s proven. It’s affordable.You’re Not Alone
Panic attacks make you feel isolated. Like no one else understands. But you’re not the only one. Millions have walked this path. And they found their way out-not by avoiding fear, but by learning how to move through it. Your plan isn’t about stopping panic forever. It’s about giving you back control. One breath. One moment. One day at a time. The next time you feel it coming, don’t fight it. Don’t run. Don’t wait. Breathe. Ground. Remember: this feeling is temporary. And you’ve got the tools to get through it.Can I stop panic attacks without medication?
Yes. Many people fully manage panic attacks using only breathing and grounding techniques. Research shows that consistent practice of these methods reduces attack frequency by up to 70% over time. Medication is helpful for some, especially early on, but it’s not required. The most effective long-term strategy combines behavioral tools with professional support like CBT.
How long does it take for breathing techniques to work?
You’ll feel calmer within 1-3 minutes of slow, deep breathing during an attack. But to build lasting change, you need daily practice. Most people see a noticeable drop in panic frequency after 2-3 weeks of doing 5-10 minutes of breathing exercises every day. Full results-like cutting attacks in half-usually take 8-12 weeks.
Are grounding techniques effective during a panic attack?
Yes. Grounding works by shifting your brain’s focus from internal fear to external reality. Studies show that using the 5-4-3-2-1 method or focusing on a single object can reduce panic intensity by 30-40% within minutes. It doesn’t stop the attack, but it makes it less overwhelming. The key is practicing it when you’re calm so it becomes automatic when you need it.
Is it safe to use Xanax for panic attacks?
Xanax (alprazolam) can be safe if used sparingly and under medical supervision. It works quickly to reduce panic symptoms within 15-30 minutes. But it carries a high risk of dependence-23% of daily users develop tolerance within 4-6 weeks. It should never be used daily or as your only tool. Reserve it for true emergencies when breathing and grounding aren’t enough.
What if I forget my plan during a panic attack?
That’s common. Most people can’t think clearly during a panic attack. That’s why you need physical reminders: write your breathing steps on a card, save a voice note saying “Breathe in 2… hold 2… out 6,” or wear a rubber band and snap it as a cue to pause and focus. The goal isn’t perfect recall-it’s having one anchor you can reach for, even when your mind is racing.
Can panic attacks come back even after I’ve mastered the plan?
Yes. Stress, sleep loss, illness, or life changes can trigger them again. But that doesn’t mean you’ve failed. It means you’re human. The difference is, now you know what to do. You don’t need to start over. Just return to your plan. Your skills are still there. You just need to use them again.